TB Stages: What They Are and How to Spot Them
When you hear "TB" most people think of a cough that just won’t go away. But tuberculosis actually moves through a few distinct stages, and knowing which stage you’re dealing with can change everything from tests to treatment.
In plain terms, TB starts when you inhale the bacteria (Mycobacterium tuberculosis). Your body either fights it off right away, or the germs hide out and stay quiet for months or years. Those are the two big buckets: primary (or active) TB and latent TB. Each bucket has its own set of signs, tests, and medication plans.
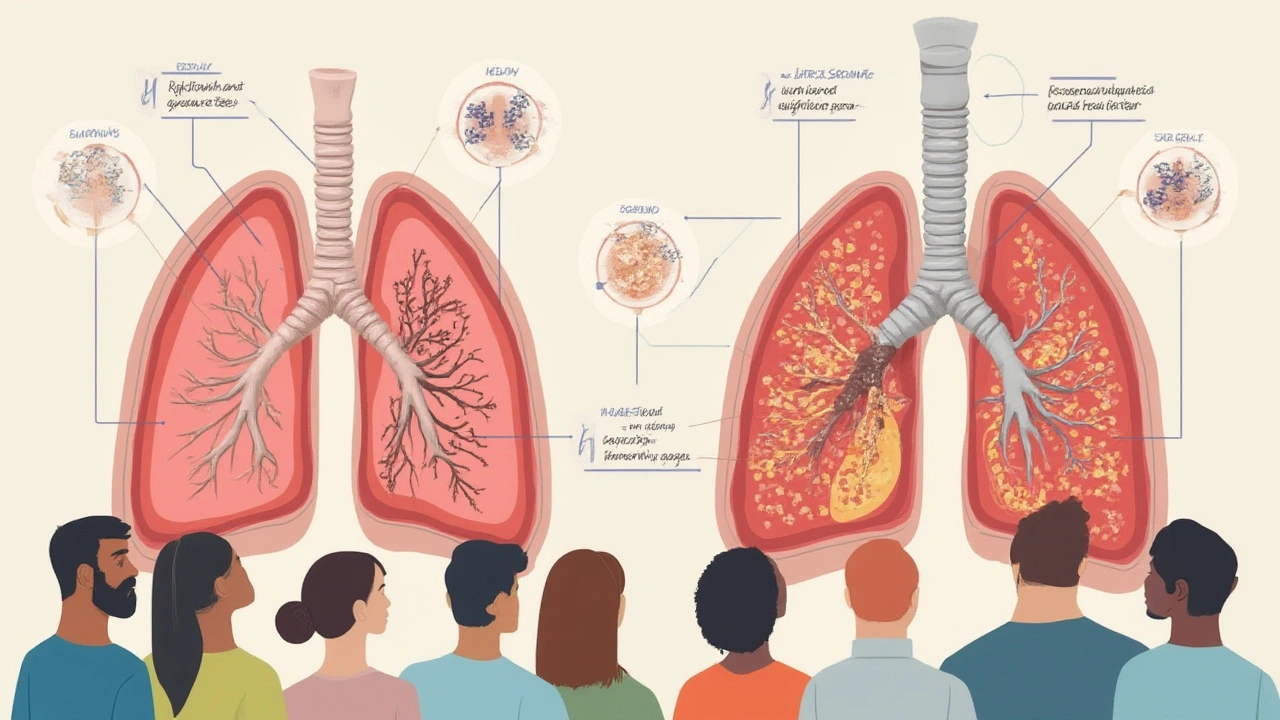
Primary vs. Latent TB
Primary (active) TB shows up with real symptoms. You might have a persistent cough, fever, night sweats, weight loss, or chest pain. The infection is doing its thing in your lungs, and it can spread to other organs if left untreated. Doctors usually catch it with a chest X‑ray, a sputum test, or a rapid molecular test that looks for TB DNA.
Latent TB is the sneaky sibling. The bacteria are alive but not causing illness. You feel fine, you don’t cough, and a standard chest X‑ray looks normal. The only clue is a positive tuberculin skin test (TST) or an interferon‑gamma release assay (IGRA). Because the germs can wake up later, doctors often recommend preventive therapy – usually a six‑month course of isoniazid or a shorter, high‑dose regimen.
Why does this matter? If you’re in the latent stage, you won’t need the full, heavy‑duty drug cocktail that active TB requires, but you still need medication to keep the infection from turning active.
How Doctors Classify TB Stages
Beyond primary and latent, clinicians break TB down further based on severity and spread:
- Early active TB: Symptoms just started, bacterial load is low, and treatment can be shorter.
- Advanced active TB: Widespread lung damage, possible involvement of other organs (like the spine or kidneys), and a longer, more intense drug regimen.
- Multidrug‑resistant TB (MDR‑TB): The bacteria resist at least isoniazid and rifampin, the two powerhouse drugs. Treatment may last 18‑24 months with second‑line meds.
- Extensively drug‑resistant TB (XDR‑TB): Even more drug resistance, requiring a very specialized treatment plan.
Doctors use a mix of lab results, imaging, and patient history to decide where you fall. A sputum smear that shows many acid‑fast bacilli pushes you into the “high bacterial load” category, while a clean smear but a positive culture suggests a lower load.
Once the stage is clear, the treatment plan follows World Health Organization (WHO) guidelines. For most drug‑sensitive active TB, it’s a six‑month regimen: two months of four drugs (isoniazid, rifampin, pyrazinamide, ethambutol) followed by four months of isoniazid and rifampin. If you’re in the latent stage, a single drug taken for a few months can be enough.
Bottom line: Knowing the TB stage helps you and your doctor pick the right tests, avoid unnecessary medication, and finish treatment successfully. If you think you’ve been exposed or you’re showing any TB‑related symptoms, get tested right away. Early detection can keep the disease from moving into a later, harder‑to‑treat stage.
Stay informed, ask questions, and keep track of your treatment milestones. TB might be a tough opponent, but understanding its stages makes it a lot easier to beat.
-
Pulmonary Tuberculosis Stages: Symptoms, Progression & Recovery Explained
Explore the stages of pulmonary tuberculosis, how it impacts the lungs, warning signs to watch for, and options for treatment and recovery in plain language.