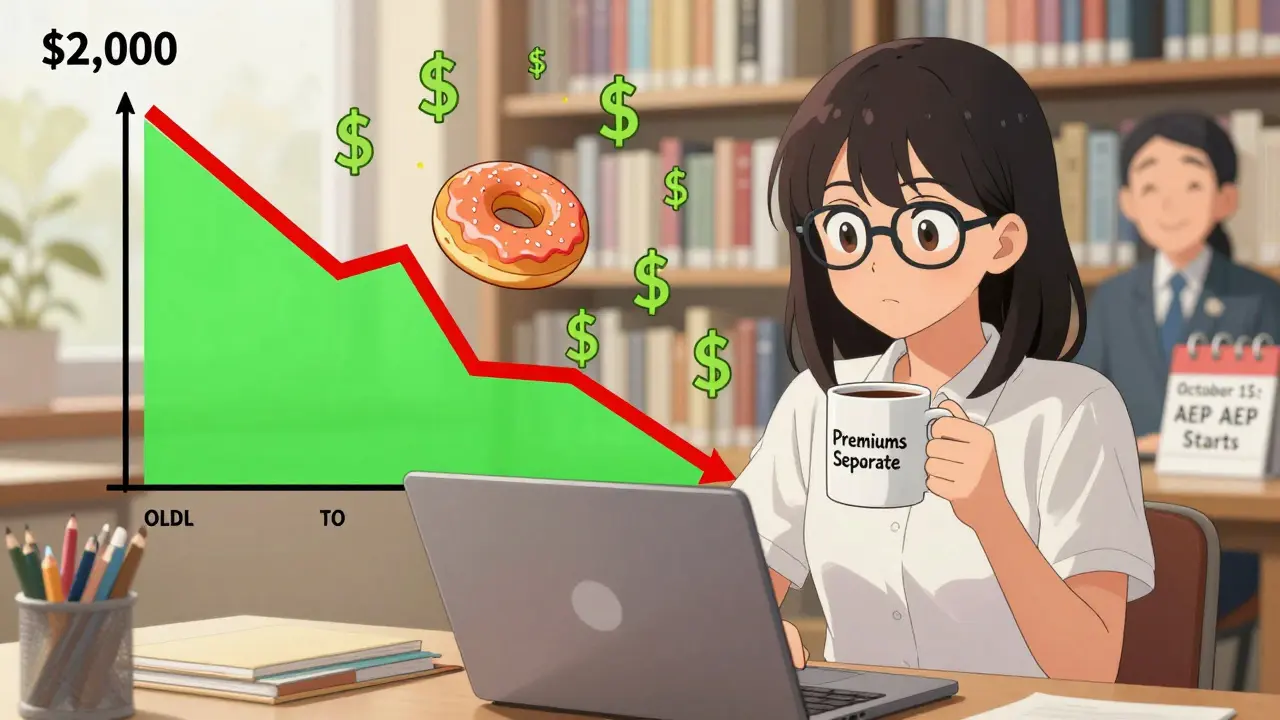
By 2025, Medicare Part D has changed more in the last two years than it has in the past 20. If you’re on Medicare and take prescription drugs, this isn’t just a tweak-it’s a complete rewrite of how you pay for them. The old system had a confusing gap called the "donut hole," where your costs would spike after you spent a certain amount. Now? That gap is gone. And for the first time, there’s a hard cap on what you pay out of pocket each year for your medications: $2,000.
What Medicare Part D Actually Covers
Medicare Part D is the part of Medicare that helps pay for prescription drugs. It’s not automatic-you have to sign up for it, either through a standalone plan (PDP) or as part of a Medicare Advantage plan (MA-PD). It covers both brand-name and generic drugs, but not every drug. Each plan has its own list, called a formulary, which tells you exactly which drugs are covered and at what cost. In 2025, every Part D plan must cover all drug classes, meaning if you need insulin, heart meds, or cancer drugs, there will be at least two options in each category. But here’s the catch: even if a drug is covered, it might be on a high-cost tier. That means you pay more. Always check if your specific medications are on your plan’s formulary before you enroll.The New Three-Phase System (No More Donut Hole)
The old Part D system had four phases: deductible, initial coverage, coverage gap (donut hole), and catastrophic coverage. That was confusing. Now, it’s simpler: three phases, and the donut hole is gone.- Deductible phase: You pay 100% of your drug costs until you hit the deductible. In 2025, that’s $590. Some plans have no deductible at all, especially those for people with low income.
- Initial coverage phase: After you meet the deductible, you pay 25% of the cost of your drugs. Your plan pays 65%, and drug manufacturers give a 10% discount on brand-name drugs. This continues until your total out-of-pocket spending (including what you and your plan paid) reaches $2,000.
- Catastrophic coverage phase: Once you hit $2,000, you pay nothing for the rest of the year. Not $5. Not $10. Nothing. The plan pays 60%, manufacturers pay 20%, and Medicare pays 20%. This is the biggest change in decades.
How Much Do You Really Pay?
The $2,000 cap sounds great, but it doesn’t include your monthly premium. That’s separate. In 2025, the average monthly premium for a standalone Part D plan is $45. For Medicare Advantage plans that include drug coverage, it’s $7. That’s a big difference. So your total cost could be $2,000 in drug costs plus $540 in premiums ($45 x 12) = $2,540. That’s still far less than what many paid before. If you take insulin, you’re protected too. The $35 monthly cap on insulin copays continues in 2025. No matter what plan you’re on, you won’t pay more than that for a month’s supply.Why Plan Choice Still Matters
Even with the $2,000 cap, not all plans are created equal. One plan might have a $0 premium but charge $100 for your blood pressure pill. Another might cost $60 a month but cover your medication at $10. Your total annual cost depends on your specific drugs, not just the premium. Most plans use a five-tier system:- Tier 1: Preferred generics (lowest cost)
- Tier 2: Generics
- Tier 3: Preferred brand-name drugs
- Tier 4: Non-preferred brand-name drugs
- Tier 5: Specialty drugs (highest cost)
Who Qualifies for Extra Help?
If your income is low, you might qualify for Extra Help (also called the Low-Income Subsidy). In 2025, 90 stand-alone Part D plans have $0 premiums for people who get Extra Help. These are called "benchmark plans" and are the cheapest option if you qualify. Extra Help also covers your deductible and reduces your copays. You don’t have to apply every year-if you’re already getting it, you’ll stay enrolled automatically.What Happens If You Don’t Enroll?
Even if you don’t take any drugs now, you should still consider signing up. If you wait and later decide you need coverage, you’ll pay a late enrollment penalty. It’s 1% of the national base premium ($35.37 in 2024) for every month you go without creditable drug coverage after your Initial Enrollment Period. That penalty sticks with you forever. Your Initial Enrollment Period is the 7 months around your 65th birthday. If you miss it and don’t have other drug coverage (like from an employer), you’ll pay the penalty. Many people think they’re fine because they’re healthy now. But medications can change fast. A diagnosis, a new condition, or even a change in your health can make you need drugs tomorrow.How to Pick the Right Plan
Don’t just pick the cheapest premium. Use the Medicare Plan Finder tool. It’s free, official, and lets you compare plans side-by-side. Here’s what to do:- Write down every drug you take, including the dose and how often you take it.
- Enter those drugs into the Plan Finder.
- Filter by your pharmacy-make sure your local pharmacy is in the plan’s network.
- Look at the total estimated cost for the year: premiums + out-of-pocket drug costs.
- Don’t assume the plan with the lowest premium is cheapest. Sometimes the plan with a $50 premium saves you $1,000 on drugs.
When Can You Change Plans?
You can switch plans once a year during the Annual Enrollment Period: October 15 to December 7. Changes take effect January 1. If you qualify for Extra Help, you can switch plans at any time. Also, if your plan changes its formulary or stops covering a drug you need, you can switch outside of enrollment season.What Experts Are Saying
The Kaiser Family Foundation says the 2025 redesign will cut average out-of-pocket spending by 40%. The Medicare Rights Center says it’s the most important change to Part D since it started. But they also warn: "The redesign doesn’t fix high drug prices-it just protects you from them." Real users say the same thing. One woman on a Medicare forum wrote: "I used to stress every month wondering if I’d hit the donut hole. Now I just pay my $35 for insulin and know I’m covered. It’s a relief." But confusion still exists. A Reddit user posted in September 2024: "I thought the $2,000 cap meant I’d pay no more than $2,000 total. I didn’t realize premiums were extra." That’s a common mistake. Always add premiums to your out-of-pocket costs when calculating your total.What’s Next?
In 2026, the $2,000 cap will rise to $2,100, and after that, it will adjust yearly with inflation. The government is also working on ways to lower drug list prices, but those changes are still years away. For now, the $2,000 cap and the elimination of the donut hole are the biggest wins for patients.Where to Get Help
You don’t have to figure this out alone.- Call 1-800-MEDICARE (1-800-633-4227). They handled 78 million calls in 2023.
- Find your local State Health Insurance Assistance Program (SHIP). They offer free, one-on-one counseling. In 2023, they helped over 5 million people.
- Use the Medicare Plan Finder tool. It’s updated daily and includes all 2025 plans.
Medicare Part D isn’t perfect. But in 2025, it’s finally working the way it was meant to: helping people afford the drugs they need without going broke.
Does Medicare Part D cover all my medications?
No. Each Part D plan has its own list of covered drugs, called a formulary. It must cover all drug classes, but not every drug within those classes. You need to check if your specific medications are covered and on which tier. A drug that’s covered by one plan might not be covered by another, or it might cost much more.
Is the $2,000 out-of-pocket cap per year or per drug?
It’s per year, and it’s for all your covered Part D drugs combined. Once you’ve spent $2,000 out of pocket on covered drugs-including what you paid during the deductible and initial coverage phases-you enter catastrophic coverage and pay nothing for the rest of the year. This includes payments made through Extra Help or other assistance programs.
Do I still have to pay a monthly premium with the new $2,000 cap?
Yes. The $2,000 cap only covers what you pay for your drugs. Your monthly premium is separate and still due every month. For example, if your premium is $45, you’ll pay $540 in premiums over the year, plus up to $2,000 for your drugs. That’s a total of $2,540, but it’s still far less than what many paid before the 2025 changes.
What if I can’t afford my Part D premium?
If your income is low, you may qualify for Extra Help (Low-Income Subsidy). This program can pay your premium, deductible, and reduce your copays. In 2025, 90 stand-alone Part D plans have $0 premiums for Extra Help enrollees. You can apply through Social Security or your state’s Medicaid office.
Can I switch Part D plans anytime?
You can normally switch only during the Annual Enrollment Period (October 15-December 7). But if you qualify for Extra Help, you can switch at any time. You can also switch if your plan drops a drug you take, raises your costs significantly, or if you move out of your plan’s service area.
What happens if I miss my Initial Enrollment Period for Part D?
If you don’t enroll when you’re first eligible and don’t have other creditable drug coverage, you’ll pay a late enrollment penalty. It’s 1% of the national base premium ($35.37 in 2024) for every month you delay. That penalty is added to your monthly premium forever, even if you enroll later. It’s best to enroll even if you don’t take drugs now.
Are generic drugs cheaper than brand-name drugs under Part D?
Yes. Most Part D plans put generics on the lowest cost tiers. You’ll pay less in copays or coinsurance for generics than for brand-name drugs. Even with the 10% manufacturer discount on brand-name drugs during initial coverage, generics are still the most affordable option. Always ask your doctor if a generic version is available.