Side Effect Tolerance Calculator
How does tolerance develop to your medication?
This tool shows you which side effects are likely to fade over time based on the medication class you're taking. Remember: tolerance to side effects doesn't mean the drug stopped working for its intended purpose.
Have you ever started a new medication and felt awful for the first few days-nausea, dizziness, fatigue-only to wake up one morning and realize those symptoms are gone? Meanwhile, that constipation or dry mouth? Still there. It’s not just in your head. This is called tolerance development, and it’s one of the most misunderstood parts of how medicines work in your body.
Why Do Some Side Effects Disappear?
Your body doesn’t just accept drugs passively. It fights back. When you take a medication regularly, your cells start adapting. Think of it like turning down the volume on a loud speaker. At first, the noise is overwhelming. But after a while, your ears adjust. The same thing happens in your brain and organs. There are three main ways your body builds tolerance. The first is through your liver. Certain medications, like barbiturates or even alcohol, tell your liver to produce more enzymes-specifically, the cytochrome P-450 family. These enzymes break down drugs faster. So over time, the same dose doesn’t stick around as long. That’s why some side effects fade: your body clears the drug before it can cause the same reaction. The second way is at the receptor level. Imagine your brain has millions of tiny locks (receptors), and the drug is the key. At first, the key fits perfectly and turns hard-causing strong effects. But after repeated use, your body starts removing some locks, making the remaining ones less sensitive, or even changing their shape so the key doesn’t fit as well. This is called pharmacodynamic tolerance. It’s why the dizziness from a new antidepressant vanishes after two weeks, but the sexual side effects don’t. The third mechanism is even more specific. Your cells can change the actual building blocks of their receptors. For example, with chronic alcohol use, the brain increases certain subunits of the NMDA receptor by up to 60%. This rewires how neurons respond, pushing the system back toward balance. It’s not just about fewer receptors-it’s about different ones.Differential Tolerance: Not All Side Effects Are Created Equal
Here’s the key insight: not all side effects develop tolerance at the same rate. This is called differential tolerance. Some systems adapt quickly. Others barely move. Take opioids. After just two or three doses, your brain starts to tolerate the sedative effects. That initial foggy feeling? Gone in a week. But your gut? It doesn’t care about brain adaptations. Constipation stays stubbornly high-up to 90% of the original intensity. That’s why doctors always prescribe laxatives with opioids from day one. They know tolerance won’t help there. Benzodiazepines work the same way. The drowsiness fades within 10-14 days. But the anxiety relief? That stays strong. That’s why people can take them for months without losing their calming effect, even though they feel less sleepy. Antidepressants like SSRIs? Nausea drops off in 2-3 weeks for 73% of users. But sexual side effects? They stick around for over half of people, sometimes permanently. Why? Because the receptors involved in digestion adapt fast. The ones tied to sexual function? Not so much. Even blood pressure meds like beta-blockers follow this pattern. The fatigue you feel at first? It fades by 65% within three months. But the drop in blood pressure? That stays steady. Your body adjusts to the tiredness, not the effect you actually need.What’s Going On in the Brain?
It’s not just about chemistry-it’s about balance. Your brain is constantly trying to keep everything stable. When a drug floods your system with serotonin, dopamine, or GABA, your brain says, “Whoa, too much.” So it cuts back. It makes fewer receptors. It changes how signals travel. It’s like a thermostat turning down the heat when it gets too warm. Dr. Lynette Daws from UT Health San Antonio explains it simply: “Tolerance happens because the brain restores balance after it’s repeatedly overstimulated.” That’s why the initial side effects-those loud, obvious reactions-fade. Your brain finds a new normal. But here’s the catch: not every system can adapt equally. The gut doesn’t have the same plasticity as the brain. The liver can ramp up enzyme production. The heart can’t just rewire its receptors overnight. So while your brain gets used to the drug’s mood effects, your digestive tract stays stuck in the original response.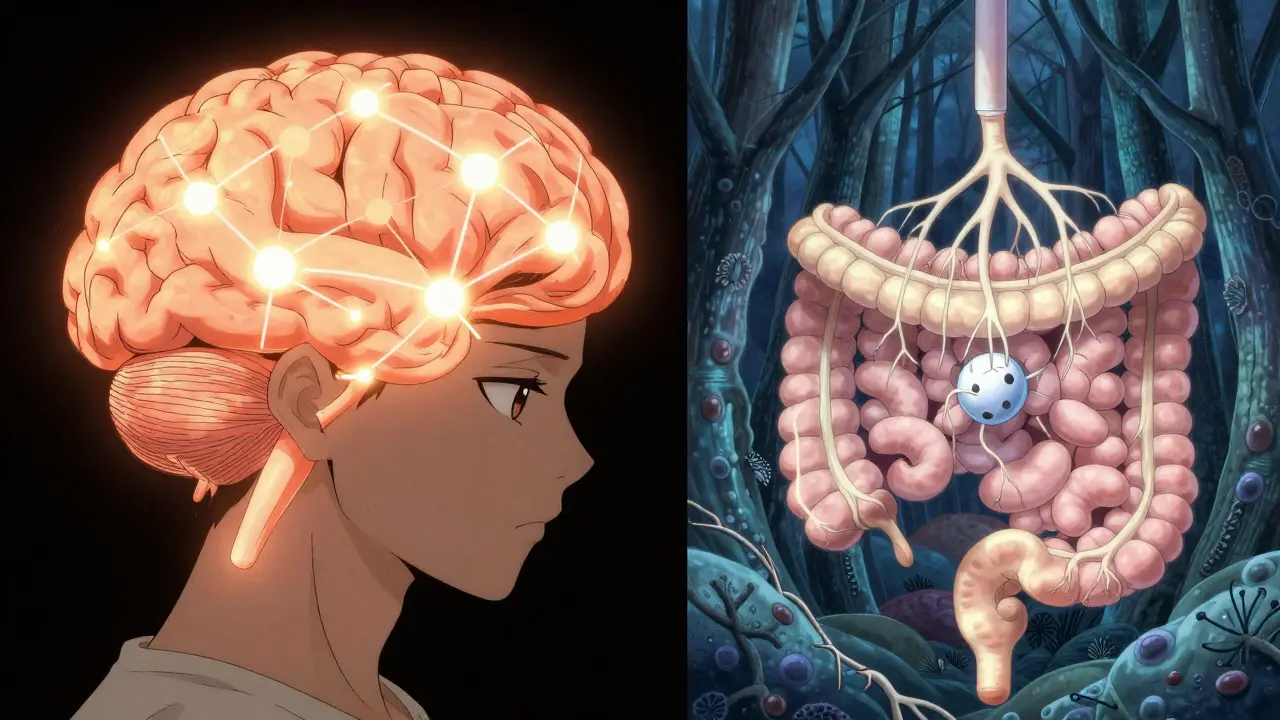
Real People, Real Experiences
You don’t need a textbook to see this. Look at what patients are saying. On Reddit, someone wrote: “Started oxycodone for back surgery-vomiting stopped after day 3, but constipation never went away.” That’s differential tolerance in action. On Drugs.com, a user taking pregabalin for nerve pain said: “The dizziness that made me fall the first week is gone. But I still get that weird numbness in my hands.” A survey of 2,145 people on SSRIs found that while 73% stopped feeling nauseous after three weeks, 58% still struggled with sexual dysfunction months later. That’s not a failure of the drug. It’s biology. These aren’t outliers. They’re the norm.Why This Matters for Your Treatment
Understanding tolerance isn’t just academic. It changes how you take your meds-and how your doctor prescribes them. If you’re on an opioid and your pain isn’t improving, your doctor might think you need a higher dose. But if your nausea and dizziness are gone, that doesn’t mean the drug isn’t working. It might mean your body just adapted to the side effects, not the pain relief. Jumping to a higher dose could increase risk without helping. Similarly, if you’ve been on an SSRI for six months and still can’t have sex, it’s not “all in your head.” It’s a known, persistent effect. Your doctor might suggest switching meds, adding another drug like bupropion, or adjusting timing-not just telling you to “wait it out.” Doctors are getting better at this. In 2022, 92% of pain specialists routinely explained differential tolerance to patients. Only 65% of primary care doctors did. That gap is closing-but you need to ask.Can You Reverse Tolerance?
Yes-but carefully. A “drug holiday”-taking a short break from the medication-can reset some tolerance. Studies on nitroglycerin (used for chest pain) showed that a 10-day break reversed 40-60% of tolerance. That’s why some patients are told to skip their patch on weekends. But this doesn’t work for everything. Stopping opioids suddenly can trigger withdrawal. Stopping antidepressants cold turkey can cause brain zaps and severe anxiety. So never quit without talking to your doctor. There’s also new science. In 2023, the FDA approved a combo drug-naltrexone and bupropion-that specifically targets opioid-induced nausea and vomiting. In trials, it cut persistent nausea by 45%. That’s not just treating symptoms. It’s attacking the root of the problem. Researchers are now working on “tolerance-resistant” drug forms. One experimental version of oxycodone, wrapped in a special polymer, showed 60% less tolerance to breathing suppression after eight weeks. That could mean safer pain control without the risk of overdose.What You Can Do
If you’re on a medication and side effects are fading-or not-here’s what to do:- Track your symptoms. Write down what you feel each week. Note when things improve or stay the same.
- Don’t assume improvement means the drug isn’t working. Tolerance to side effects ≠ loss of effectiveness.
- Ask your doctor: “Is this side effect supposed to go away? If not, why?”
- Don’t increase your dose on your own. Higher doses can worsen tolerance and increase risks.
- Know your genetics. About 7-10% of white people have a gene variant that makes them poor metabolizers of codeine. That means it won’t work for them at all. Testing is available.
The Bigger Picture
By 2030, most new brain-targeting drugs will be designed with tolerance in mind. Personalized medicine-using your genes to predict how you’ll respond-is becoming standard. That means someday, your doctor might say: “Based on your DNA, you’re likely to develop fast tolerance to drowsiness but not constipation. We’ll start you on a laxative right away.” This isn’t science fiction. It’s already happening in clinics that use tools like Epic’s tolerance prediction system, which cut unnecessary dose increases by 34% in a 12,000-patient study. Tolerance isn’t a flaw. It’s a feature of biology. Your body is trying to protect you. The trick is knowing which side effects are temporary-and which ones need a different plan. If your nausea disappeared but your constipation didn’t? That’s normal. If your anxiety improved but your sleep didn’t? That’s common. If your fatigue faded but your blood pressure stayed low? That’s working as intended. You’re not broken. You’re adapting.Why do some side effects go away but others don’t?
Different parts of your body adapt at different speeds. Your liver can speed up drug breakdown, your brain can reduce receptor sensitivity, and your gut might not adapt at all. Side effects tied to fast-adapting systems (like dizziness or nausea) fade quickly. Those tied to slower systems (like constipation or sexual dysfunction) often stick around.
Does tolerance mean my medication isn’t working anymore?
No. Tolerance to side effects doesn’t mean the drug lost its main effect. For example, opioids lose their sedative effect quickly but still relieve pain. SSRIs lose nausea but often keep helping with depression. Always check with your doctor before assuming the drug isn’t working.
Can I stop taking my medication to reset tolerance?
Sometimes-but only under medical supervision. Stopping opioids or antidepressants suddenly can cause serious withdrawal. A short break (a “drug holiday”) can help with some drugs like nitroglycerin, but it’s risky for others. Never quit without talking to your doctor first.
Are some people more likely to develop tolerance than others?
Yes. Genetics play a big role. About 7-10% of Caucasians have a gene variant (CYP2D6 poor metabolizer) that affects how they process codeine and other drugs. Others may have receptor variations that make them more or less sensitive. This is why two people on the same dose can have completely different experiences.
Is tolerance the same as addiction?
No. Tolerance means your body needs more to get the same effect. Addiction involves compulsive use despite harm. You can have tolerance without addiction-like someone on long-term pain meds who takes their dose as prescribed. But tolerance can be a stepping stone to dependence, so it’s important to monitor and manage it with your doctor.
What new treatments are being developed to manage tolerance?
New drugs like naltrexone-bupropion are designed to block specific side effects (like nausea) without reducing pain relief. Researchers are also testing polymer-coated pills that release drugs slowly to reduce tolerance development. In the future, genetic testing may help doctors pick the right drug and dose for you from the start.
