Many people hear a ringing, buzzing, or hissing sound in their ears when no one else does. That’s tinnitus. While it’s often linked to aging or loud noise, medications are a surprisingly common cause-and one that’s easy to miss. If you started a new pill recently and now your ears won’t stop ringing, you’re not imagining it. More than 600 prescription and over-the-counter drugs can trigger or worsen tinnitus. The good news? In many cases, it’s reversible. The key is knowing which drugs to watch for and what to do next.
How Medications Cause Ringing in the Ears
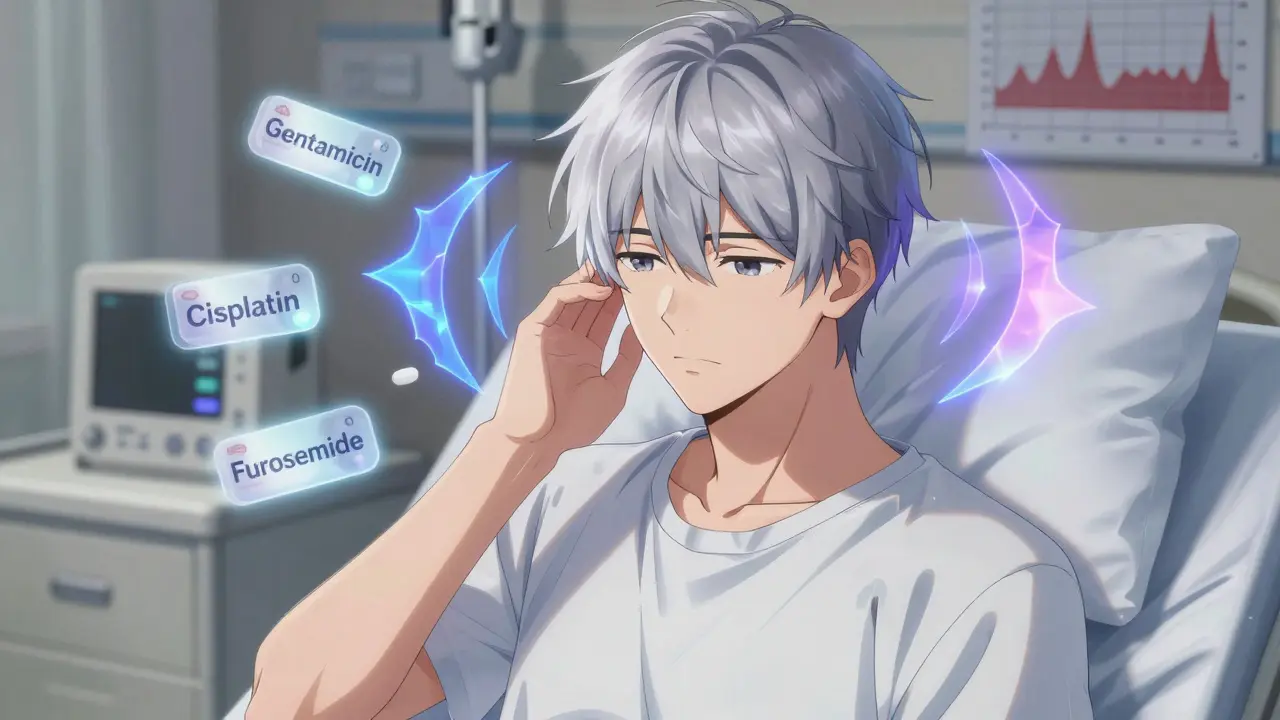
Tinnitus from medication happens because some drugs damage the inner ear. This is called ototoxicity. The inner ear doesn’t just help you hear-it also controls balance. When a drug messes with the tiny hair cells or nerves there, your brain starts misfiring. It hears sounds that aren’t there. The exact mechanism isn’t fully understood, but it’s likely tied to changes in how electrical signals travel from the ear to the brain. This isn’t rare. About 5-10% of all tinnitus cases are linked to medications, according to clinical data from 2025.
Some drugs cause tinnitus quickly-within hours or days. Others take weeks or even months. The damage can be temporary or permanent. It depends on the drug, the dose, how long you’ve been taking it, and even your genetics. Some people are just more sensitive.
Drugs Most Likely to Cause Tinnitus
Not all medications carry the same risk. Some are high-risk, others are rare offenders. Here’s what the evidence shows:
- Aminoglycoside antibiotics (like gentamicin and tobramycin): These are used for serious infections. They’re among the most dangerous. Up to 25% of people on long-term IV treatment develop permanent hearing loss or tinnitus. Topical versions (eye drops, creams) are much safer.
- Cisplatin and other chemotherapy drugs: Used for cancer, cisplatin causes ototoxicity in 30-70% of patients. Hearing loss often starts with high-pitched sounds you can’t hear anymore-like birds chirping or a microwave beep-before it affects speech.
- Loop diuretics (like furosemide): Used for fluid buildup from heart or kidney issues. High doses or fast IV administration can cause temporary ringing. It usually goes away after stopping, but not always.
- High-dose aspirin: You need to take over 4,000 mg daily for this to happen. That’s way more than a regular headache pill. Modern aspirin doses (325-650 mg) rarely cause tinnitus. But a tiny number of people are extra sensitive-even low doses can trigger it.
- NSAIDs (ibuprofen, naproxen): High doses (like 800 mg three times a day) can cause ringing, especially if taken for days. One Reddit user reported tinnitus after taking 800 mg ibuprofen for dental pain. Symptoms vanished within a week after stopping.
- Quinine: Found in some malaria drugs and tonic water. Tinnitus can appear within 24-72 hours. It usually clears up in 1-2 weeks after quitting.
- Isotretinoin (Accutane): Used for severe acne. Tinnitus is listed as a rare side effect, but some users report it. Estimates vary from less than 1% to around 5%.
- Benzodiazepines (like Xanax, Valium): Long-term use (6+ months) is linked to tinnitus in some users. Stopping them can also trigger ringing in a few cases.
- Antidepressants: Rare. Less than 1% of users report tinnitus. Some cases are tied to stopping SSRIs like sertraline (Zoloft), not starting them.
Is Your Tinnitus Reversible?
Here’s the hopeful part: about 60% of medication-induced tinnitus cases go away after you stop the drug. That’s true for NSAIDs, diuretics, aspirin, and even quinine. But not all drugs are so forgiving.
Aminoglycosides and cisplatin can cause permanent damage. Once the hair cells in your inner ear die, they don’t come back. That’s why doctors monitor hearing during treatment. If you’re on one of these drugs, you should have a baseline hearing test before starting, and follow-ups every 1-2 weeks.
Timing matters too. Most people notice ringing within the first two weeks of starting the drug. But some drugs-especially certain antibiotics or chemo agents-can cause delayed reactions up to 90 days later. So if you started a new medication three months ago and now your ears are ringing, don’t rule it out.

What to Do If You Think a Medication Is Causing Your Tinnitus
Stop taking the drug? No. Never do that on your own. That’s dangerous. Instead:
- Write down the details: What medication? When did you start? What dose? When did the ringing begin? Did anything else change?
- Call your doctor: Don’t wait. Say, “I’ve started ringing in my ears since I began [drug name].” Bring your list. Your doctor may check your kidney function or drug levels-especially if you’re on a high-risk medication.
- Ask about alternatives: Can the dose be lowered? Is there another drug with less risk? For example, if you’re on furosemide for fluid retention, maybe a different diuretic works just as well.
- Don’t panic about aspirin: If you take 81 mg daily for heart health, tinnitus is extremely unlikely. Don’t quit without talking to your doctor.
- Consider a hearing test: Even if the ringing fades, a baseline audiogram helps track changes. Audiologists can spot early signs of damage you can’t feel.
What Doesn’t Cause Tinnitus
There’s a lot of misinformation out there. Let’s clear it up:
- Antidepressants: They’re rarely the culprit. If you’re on an SSRI and have tinnitus, it’s more likely due to stress, noise exposure, or another medication.
- Acetaminophen (Tylenol): No strong evidence links it to tinnitus. It’s considered safe for hearing.
- Statins: Cholesterol drugs like atorvastatin don’t cause ringing. Some studies even suggest they may protect hearing.
- Caffeine: While some people swear it makes their tinnitus worse, studies show no direct link. Cutting caffeine won’t fix it.
How Doctors Monitor for Ototoxicity
For high-risk drugs, there are protocols in place. Hospitals are getting better about this. As of 2023, 68% of major U.S. hospitals now use therapeutic drug monitoring for ototoxic medications-up from 45% in 2018.
Here’s what that looks like:
- Baseline hearing test: Done before treatment starts. This records your hearing at all frequencies.
- Regular check-ups: Every 1-2 weeks during treatment for drugs like cisplatin or gentamicin.
- Blood tests: To check drug levels and kidney function. Poor kidney clearance means more drug in your system-higher risk.
- Genetic testing: Emerging. Some people have gene variants that make them far more sensitive to ototoxic drugs. This isn’t routine yet, but it’s coming.
Still, only 35% of primary care doctors routinely screen for ototoxicity risk before prescribing. That’s why you need to speak up. If you’re on a high-risk drug, ask: “Should I get my hearing checked?”

What If You Can’t Stop the Medication?
Sometimes, the drug is essential. You need it to survive. Chemo. Antibiotics for a life-threatening infection. In those cases, you can’t just quit. But you can still manage the tinnitus.
Sound therapy-using white noise, fans, or apps-helps 60-70% of people cope better. Cognitive behavioral therapy (CBT) for tinnitus reduces the emotional distress. It doesn’t silence the sound, but it stops it from controlling your life. These don’t fix the cause, but they make living with it possible.
The Bigger Picture
Over 50 million Americans have tinnitus. A small fraction of those cases come from medications. But because so many people take pills daily, even a rare side effect adds up. The cost? Around $2.7 billion a year in the U.S. for tinnitus-related care.
Researchers are working on solutions. The NIH just funded $12.5 million to study otoprotective agents-drugs that shield the ear without affecting the treatment. Clinical trials are underway. In the future, you might get a protective shot before chemo.
For now, awareness is your best defense. Know the drugs. Track your symptoms. Talk to your doctor. And remember: if tinnitus started after a new medication, it’s likely related. You’re not alone. And you’re not crazy. There’s a reason-and a way forward.
Can aspirin cause ringing in the ears?
Yes, but only at very high doses-over 4,000 mg daily. That’s more than 12 regular aspirin tablets. Most people take 325-650 mg for headaches or heart health, and that’s not linked to tinnitus. A tiny number of individuals are unusually sensitive and may hear ringing at lower doses, but this is rare.
Is tinnitus from medication permanent?
It depends on the drug. For most common offenders like NSAIDs, diuretics, or aspirin, tinnitus is reversible once you stop the medication. But with aminoglycoside antibiotics (like gentamicin) and chemotherapy drugs like cisplatin, damage can be permanent. The inner ear’s hair cells don’t regenerate. Early detection and stopping the drug fast can prevent permanent loss.
Can antidepressants cause tinnitus?
Rarely. Less than 1% of users report tinnitus from antidepressants. Some cases are linked to stopping the drug (like sertraline/Zoloft), not starting it. If you’re on an SSRI and develop ringing, it’s more likely due to stress, noise exposure, or another medication. Don’t assume it’s the antidepressant without checking with your doctor.
Should I stop taking my medication if I get tinnitus?
No. Never stop a prescribed medication on your own. Some drugs are life-saving. Instead, contact your doctor right away. They can assess whether the drug is likely the cause, check your hearing or kidney function, and possibly switch you to a safer alternative. Your health depends on this conversation.
Can hearing tests detect medication-induced tinnitus early?
Yes. A baseline audiogram before starting a high-risk drug can catch early hearing changes. Ototoxic damage often starts with loss of high-frequency sounds-like birdsong or a microwave beep-before it affects speech. Regular hearing tests during treatment (every 1-2 weeks) can catch this before it becomes permanent. Many hospitals now require this for chemo and aminoglycoside therapy.
Next Steps
If you’re on a medication and notice new ringing in your ears:
- Write down the drug name, dose, and when the ringing started.
- Call your prescribing doctor within 48 hours.
- Ask: “Could this be ototoxicity? Should I get a hearing test?”
- Don’t change your dose or stop the drug without medical advice.
- If you’re on chemo, antibiotics, or diuretics, insist on regular hearing checks.
Medication-induced tinnitus is preventable. You just need to know the signs-and speak up before it’s too late.