What Exactly Is Ringworm?
Don’t let the name fool you-ringworm has nothing to do with worms. It’s a fungal infection, plain and simple. The real name is tinea, and it’s caused by mold-like fungi called dermatophytes that live on the outer layers of skin, hair, and nails. These fungi don’t burrow deep; they feed on keratin, the protein that makes up your skin, hair, and nails. That’s why they thrive in warm, sweaty places like between your toes, under your armpits, or on your scalp.
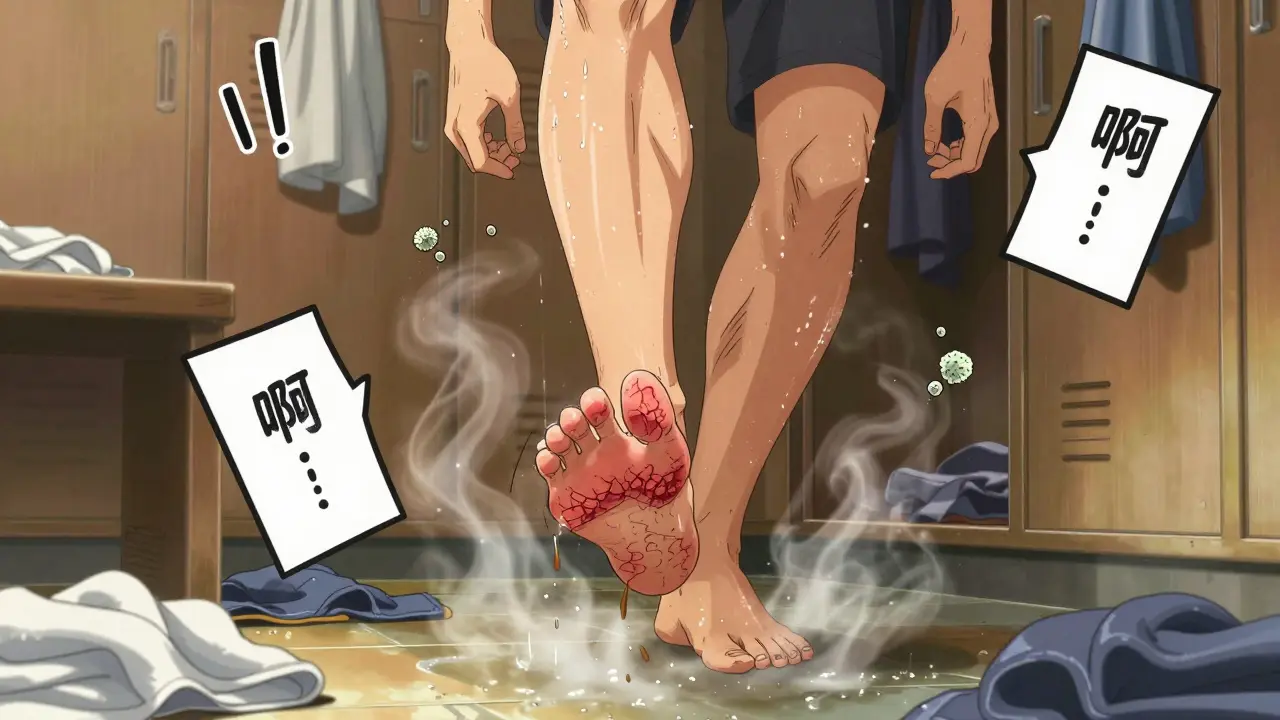
The classic sign? A red, circular rash with a raised, scaly edge and a clearer center. It looks like a ring-that’s where the name came from. But not all cases look like that. Sometimes it’s just a patch of red, itchy skin that doesn’t form a perfect circle. In kids, it can show up as flaky, bald spots on the scalp. On the feet, it peels and stings. On the groin, it burns. And on the nails, it turns them thick, yellow, and crumbly.
According to the CDC, about 20-25% of people worldwide will get ringworm at some point. In the U.S. alone, there are around 40 million cases every year. That’s more than 1 in 8 people. And it’s not rare in Durban or anywhere else with warm, humid weather. If you’ve ever walked barefoot in a gym shower or shared a towel with someone who had it, you’ve put yourself at risk.
Types of Tinea: Where It Shows Up and What It Looks Like
Ringworm isn’t one thing-it’s many. The type you get depends on where the fungus lands. Here’s what to watch for:
- Tinea corporis (body ringworm): The textbook case. Red, itchy, ring-shaped rash on arms, legs, or torso. Starts small, about the size of a coin, and grows outward. The edges are raised and scaly; the middle clears up. It’s the most common type in adults.
- Tinea pedis (athlete’s foot): Affects the feet, especially between the toes. Skin peels, cracks, and smells bad. It burns when you sweat. This is the #1 reason people visit dermatologists in summer. About 15% of all ringworm cases are this kind.
- Tinea cruris (jock itch): Red, itchy patches on the inner thighs, groin, or buttocks. Worse in men, but women get it too, especially if they wear tight clothes or sweat a lot. Makes up about 20% of adult cases.
- Tinea capitis (scalp ringworm): Mostly in kids under 10. Starts as a small scaly patch that grows. Hair falls out in chunks. Sometimes it turns into a swollen, pus-filled lump called a kerion-this can scar the scalp permanently if not treated fast.
- Tinea unguium (nail fungus): Toenails are hit three times harder than fingernails. Why? Shoes create the perfect warm, dark, damp environment. Nails get thick, yellow, brittle. They can break off easily. It’s slow to develop but even slower to fix.
Incubation time? Usually 4 to 14 days after exposure. But sometimes it takes up to three weeks. That’s why people think they caught it from the gym last week-when really, it was from their dog three weeks ago.
How Do You Catch It?
You don’t need to be dirty to get ringworm. You just need to be in the wrong place at the wrong time. The fungi live on surfaces. They survive on towels, shower floors, wrestling mats, combs, even pet fur.
Here’s how most people catch it:
- Skin-to-skin contact (60% of cases): Hugging, wrestling, sharing a bed with someone who has it.
- Contaminated surfaces (30%): Walking barefoot in a locker room, using a towel someone else used, sitting on a gym bench.
- Animals (10%): Cats and dogs-especially puppies and kittens-are common carriers. If your pet has a patch of missing fur or flaky skin, it might be ringworm. Vets say 15-20% of animal handlers get infected.
Some things make you way more likely to get it:
- Wearing tight shoes and sweaty socks all day
- Having hyperhidrosis (excessive sweating)-affects 3% of people
- Playing contact sports like wrestling-84% of high school wrestlers have had it at least once
- Not wearing flip-flops in public showers-this increases your risk by 45%
And here’s the kicker: if you’re immunocompromised-due to diabetes, HIV, or chemotherapy-you’re 3.5 times more likely to have trouble clearing the infection. It doesn’t just stick around longer; it spreads faster.
Top Antifungal Creams That Actually Work
For most skin and body ringworm, you don’t need a prescription. Over-the-counter creams work fine-if you use them right.
Here are the most effective active ingredients, backed by clinical studies:
- Clotrimazole (1%): Works in 70-80% of cases. Needs 2-4 weeks of twice-daily use. Cheaper, but slower.
- Miconazole (2%): Slightly less effective at 65-75%. Good for mild cases.
- Terbinafine (1%): The gold standard. Works in 80-90% of cases. Often clears symptoms in just 3-5 days. Treatment time? Only 1-2 weeks. Amazon reviews show 82% of users rate it highly.
- Ketoconazole (2%): 75-85% effective. Often found in medicated shampoos too, useful for scalp or body.
Apply it right: Clean and dry the area first. Put the cream on the rash and a little beyond the edges-about a finger’s width outside. That’s because the fungus spreads invisibly. Do it twice a day, every day. No skipping.
Most people stop when the redness fades. Big mistake. The fungus is still alive under the skin. That’s why 45% of people get it back. You need to keep applying until the full 2-4 weeks are done-even if it looks perfect.
When Creams Aren’t Enough: Oral Medications
Topical creams won’t cut it for scalp or nail infections. The fungus hides too deep. For tinea capitis, you need oral terbinafine-250mg daily for 4 to 6 weeks. Cure rates? 85-90%. For nail fungus, it’s the same drug, but for 6 to 12 weeks. It’s not fun-side effects can include stomach upset or headaches-but it’s the only way to get rid of it.
Prescription oral antifungals cost $25 to $150 depending on insurance. Over-the-counter creams? $5 to $15 per tube. That’s why most people try creams first. But if you’ve tried for 2 weeks and it’s spreading, don’t wait. See a doctor. Delayed treatment means the rash can cover 30-50% more skin in just two weeks.
Dr. Adam Friedman from George Washington University says starting treatment early can cut healing time by 5 to 7 days. That’s the difference between being back to normal by Friday or still itching next week.
Why Some Treatments Fail
Not everyone gets better. About 10-15% of cases don’t respond to standard treatment. Why?
- Stopping too soon: 68% of Reddit users admit they quit once the rash looked better. Bad move.
- Wrong product: Using an antifungal for athlete’s foot on scalp ringworm won’t work. The fungi are different.
- Resistant strains: A 2022 study found terbinafine-resistant ringworm strains are rising-up 12% since 2018. It’s not common yet, but it’s happening.
- Reinfection: You treated your skin but not your socks, shoes, or bed sheets. The fungus comes back.
And natural remedies? Tea tree oil gets promoted a lot. But a 2021 Cochrane Review found it clears the infection in only 40-50% of cases. That’s half as good as clotrimazole. Don’t waste time on it if you want results.

Prevention: Stop It Before It Starts
Ringworm is easy to catch, but even easier to prevent.
- Wear flip-flops in showers, pools, and locker rooms. Reduces risk by 45%.
- Change socks daily. If you sweat a lot, change them twice.
- Don’t share towels, combs, or hats. That cuts transmission by 30%.
- Keep skin dry. After showers, pat dry-especially between toes and under breasts.
- Check your pets. If your cat has bald patches, take it to the vet. Don’t assume it’s just shedding.
- Wash gym clothes after every use. Fungi live in fabric.
And if someone in your house has it? Wash their bedding, towels, and clothes in hot water. Dry on high heat. Vacuum carpets and wipe down shared surfaces with bleach or antifungal spray.
The Hidden Cost: Social and Emotional Impact
Ringworm isn’t just a skin problem. For teens and kids, it’s a social nightmare. A 2022 Kids Health survey found 73% of adolescents with visible ringworm were bullied or avoided by peers. One kid told me he was sent home from school for two weeks because the teacher thought it was contagious in a scary way-even though it’s not life-threatening.
Adults feel it too. Men with jock itch avoid the gym. Women with scalp ringworm hide under hats, even in summer. The stigma is real. And it makes people delay treatment longer than they should.
Remember: ringworm is common. It’s not dirty. It’s not your fault. It’s just a fungus that got lucky.
What to Do If It Doesn’t Go Away
If you’ve used an antifungal cream for 2 weeks with no improvement, or if the rash is spreading, getting worse, or forming blisters or pus, see a doctor. You might need:
- A skin scraping to confirm it’s fungal (not eczema or psoriasis)
- A stronger prescription cream or oral medication
- Testing for underlying conditions like diabetes or a weakened immune system
And if you’re treating a child with scalp ringworm-don’t wait. Get help fast. Kerion can cause permanent hair loss.
Is ringworm contagious?
Yes, ringworm is very contagious. It spreads through direct skin contact, sharing towels or clothing, or touching surfaces like gym mats or shower floors where the fungus lives. It can also spread from infected pets like cats and dogs.
Can I use the same antifungal cream for athlete’s foot and body ringworm?
Yes, most over-the-counter antifungal creams like clotrimazole or terbinafine work for both. The key is applying it correctly-on the rash and a bit beyond the edges. But if you have scalp or nail ringworm, you’ll need different treatment-usually oral medication.
How long does it take for antifungal cream to work?
You’ll usually see improvement in 3 to 7 days, but you need to keep using it for 2 to 4 weeks total. Stopping early is the #1 reason ringworm comes back. Even if it looks gone, the fungus may still be under the skin.
Can ringworm cause permanent damage?
In rare cases, yes. Scalp ringworm can lead to a painful, swollen lump called a kerion, which can scar the scalp and cause permanent hair loss if untreated. Nail infections can permanently thicken or deform nails. Early treatment prevents this.
Is ringworm more common in children?
Yes, especially scalp ringworm (tinea capitis). About 60% of all scalp cases happen in children under 10. They’re more likely to get it from pets or school outbreaks. Adults usually get body or foot ringworm.
Do I need to throw away my shoes if I have athlete’s foot?
No, but you should disinfect them. Spray the inside with antifungal spray or wipe with a vinegar solution. Let them air out for 24 hours. Rotate shoes so each pair has time to dry completely. Fungus thrives in damp, dark spaces.
