When a doctor prescribes a biosimilar instead of the original biologic drug, the billing process isn’t as simple as switching one pill for another. Unlike generic small-molecule drugs, biosimilars are complex biological products made from living cells. That complexity carries over into how they’re coded, billed, and paid for-especially under Medicare Part B, which covers drugs given in clinics and doctor’s offices. If you’re a provider, pharmacist, or even a patient trying to understand why your bill looks different, the system can feel confusing. But once you break it down, it’s not as complicated as it seems.
How Biosimilars Are Different from Generics
First, you need to understand the big difference between generics and biosimilars. A generic version of a drug like metformin is chemically identical to the brand-name version. The FDA can approve it based on chemical tests and bioequivalence studies. Biosimilars? They’re not identical. They’re highly similar to the original biologic-like Humira or Enbrel-but made using living cells, so tiny variations are unavoidable. That’s why they need their own clinical trials and can’t be automatically substituted like generics.
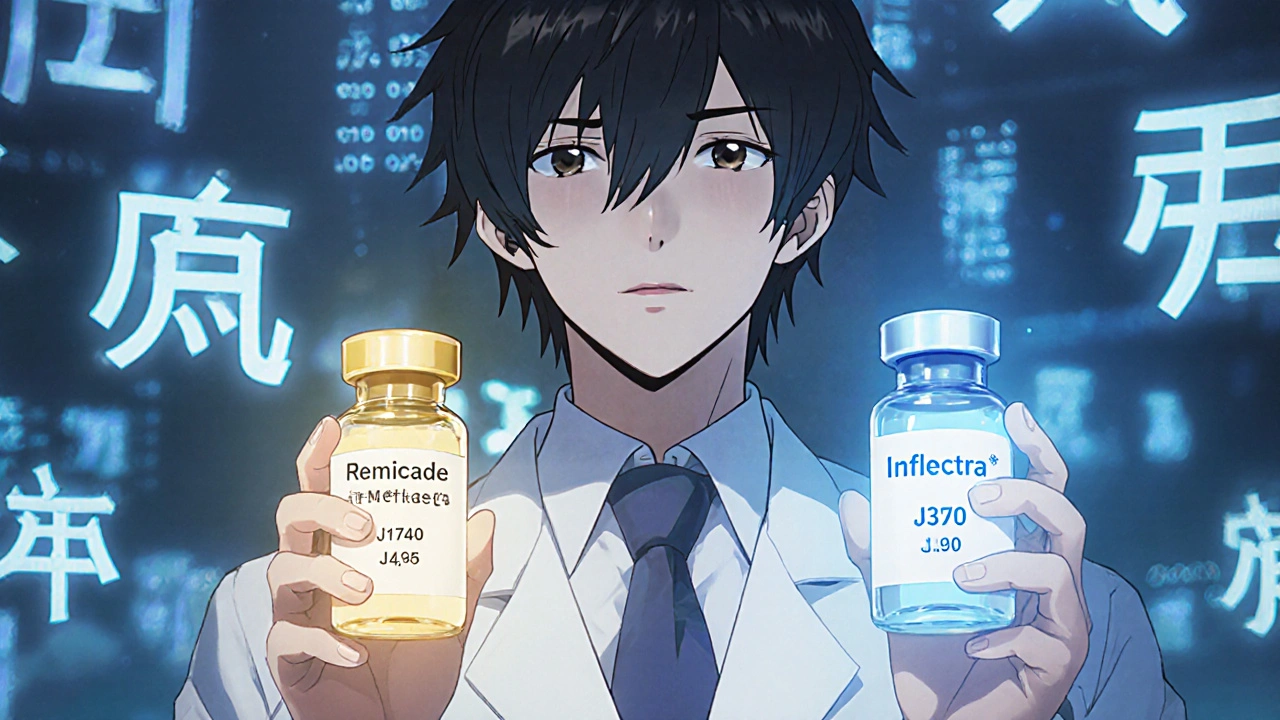
This difference matters for billing. Generics use the same HCPCS code as the brand drug. But each biosimilar gets its own unique code. That means if your clinic gives you Inflectra (a biosimilar to Remicade), they can’t just bill it as Remicade. They have to use the exact code for Inflectra. This system was put in place in 2018 to make sure each biosimilar is tracked and paid for based on its own price-not a mix of all biosimilars in the same class.
The Coding System: Q-Codes and J-Codes
Every FDA-approved biosimilar gets a specific HCPCS code. These are either temporary Q-codes or permanent J-codes. For example:
- Inflectra (infliximab-abda) → J1745
- Renflexis (infliximab-abda) → J1747
- Amjevita (adalimumab-atto) → J3590
Before 2018, all infliximab biosimilars shared one code: Q5101. That created a problem. If one company launched a biosimilar at a lower price, others could ride on the same payment rate without lowering their own prices. It was like letting a cheaper car get the same gas subsidy as an expensive one. The 2018 change fixed that. Now, each biosimilar has its own code and its own payment rate.
These codes are updated quarterly by CMS. If your clinic uses an outdated code, claims get denied. That’s why many practices now keep a printed or digital copy of the latest CMS drug pricing file handy. One oncology practice in Ohio reported a 40% drop in claim denials after they started checking the CMS website every month instead of quarterly.
How Payment Is Calculated
Medicare Part B pays providers 106% of the Average Selling Price (ASP) for most drugs. For biosimilars, that means:
- 100% of the biosimilar’s own ASP
- Plus 6% of the reference product’s ASP
So if Remicade (the reference drug) costs $2,500 per dose and Inflectra costs $2,000, here’s what the provider gets paid:
- 100% of Inflectra’s ASP: $2,000
- Plus 6% of Remicade’s ASP: $150
- Total reimbursement: $2,150
That $150 add-on is the same whether you give the reference drug or the biosimilar. That’s the catch. Even though Inflectra costs $500 less, the provider only saves $30 in profit per dose ($150 vs $150). That’s not enough to motivate many clinics to switch, especially when patients and insurers don’t always notice the cost difference.
Dr. Mark Trusheim from MIT calculated that this structure gives providers a financial incentive to stick with the more expensive drug. For high-volume biologics, that adds up. One rheumatology clinic in Texas found they made $18,000 more per year by sticking with Remicade instead of switching to Inflectra-even though the biosimilar cost them $100,000 less in drug purchase.

The JZ Modifier: A New Layer of Complexity
Starting July 1, 2023, CMS added another layer: the JZ modifier. This is required on claims for infliximab and its biosimilars when no drug is discarded. That means if a vial contains 100 mg and you only use 50 mg, you must document that you didn’t waste the rest. If you did waste it, you don’t use the JZ modifier.
Why? Because Medicare wants to avoid overpayment. But it’s created a headache for providers. A gastroenterology practice in Atlanta said their billing staff now spends 30% more time verifying vial sizes and documenting waste. One nurse said they now have to take a photo of the vial before and after use just to make sure they’re compliant. That’s not clinical work-it’s paperwork.
Manufacturers like Fresenius Kabi have stepped in with free coding guides and webinars. Their 2023 guide for STIMUFEND® was rated "helpful" by 87% of surveyed providers. But that’s still a patchwork solution. There’s no central, easy-to-use CMS tool that tells you exactly which code to use, what modifier to add, and what the current ASP is-all in one place.
Why Adoption Is Still Low in the U.S.
Even though 32 biosimilars are approved in the U.S. as of late 2023, market share is stuck around 35% for most products. In Europe, it’s 75-85%. Why the gap?
It’s not just about price. It’s about payment structure. European countries use reference pricing-meaning the government sets one payment rate for all drugs in a class. Providers get the same reimbursement whether they give the brand or the biosimilar. That removes the profit incentive to stick with the expensive drug.
In the U.S., the 6% add-on tied to the reference product’s price creates a hidden disincentive. A 2022 study by Avalere Health estimated that if CMS removed the reference product’s ASP from the biosimilar payment calculation, adoption would jump by 15-20 percentage points. That’s not theoretical-it’s measurable.
MedPAC, the advisory group to Congress, has proposed a "consolidated billing" system: one payment rate for all biosimilars and the reference product, based on the lowest-cost option. That’s what Europe does. But CMS hasn’t moved yet. The agency says it’s monitoring ASP trends and may propose changes by 2025.

What Providers Need to Do Right Now
If you’re managing a clinic or pharmacy, here’s what you need to do today:
- Keep the latest CMS drug pricing file open on your computer. Update it every quarter.
- Train your billing team on the correct HCPCS codes for each biosimilar you use. Don’t assume they know.
- Implement a double-check system: pharmacist confirms the drug given, biller confirms the code used.
- For infliximab products, always check if the JZ modifier applies. Document vial usage.
- Ask your biosimilar manufacturer for their coding guide. Most offer them free.
One cancer center in Michigan reduced claim denials from 14% to under 3% by doing exactly this. They didn’t need new software. Just better habits.
What’s Next for Biosimilar Billing?
Looking ahead, two big changes could come by 2025:
- Least Costly Alternative (LCA) Payment: CMS may start paying 106% of the average price of all drugs in a class-not the reference product’s price. This would make biosimilars more attractive.
- Fixed Add-On: Instead of 6% of the reference drug’s price, CMS might set a flat $50 add-on per dose. That would remove the incentive to use expensive drugs.
These aren’t just ideas. MedPAC recommended them in June 2023. CMS has already asked for public feedback. If you’re in healthcare, this is a moment to pay attention. Policy changes could reshape how biosimilars are used-and who profits.
Right now, the system rewards complexity over simplicity. But as more biosimilars enter the market, pressure will grow to fix it. The goal should be clear: lower costs for patients, fair payment for providers, and real competition-not just the illusion of it.
Do biosimilars use the same HCPCS code as the reference biologic?
No. Each biosimilar has its own unique HCPCS code-either a Q-code (temporary) or J-code (permanent). The reference biologic keeps its own code. For example, Remicade uses J1740, while Inflectra uses J1745. This change started in 2018 to ensure accurate payment for each product.
Why do providers sometimes prefer the brand biologic over the biosimilar?
Because Medicare Part B pays providers 106% of the reference product’s ASP for both the brand and the biosimilar. So if the biosimilar costs $500 less per dose, the provider’s profit difference is only about $30 per dose-too small to justify switching, especially when patients don’t see a difference in out-of-pocket cost. The current payment structure doesn’t reward cost savings.
What is the JZ modifier and why is it required?
The JZ modifier is required on claims for infliximab and its biosimilars when no drug is discarded from the vial. It tells Medicare the provider used the entire vial and didn’t waste any. If you discard even a small amount, you don’t use JZ. This rule started July 1, 2023, to prevent overpayment, but it’s added significant documentation burden for clinics.
How often are biosimilar payment rates updated?
CMS updates biosimilar payment rates quarterly, based on the Average Selling Price (ASP) data submitted by manufacturers. The most recent update was July 1, 2023. Providers must check the CMS website or their manufacturer’s coding guide each quarter to avoid claim denials.
Is the U.S. biosimilar market growing faster than Europe’s?
No. As of 2023, U.S. biosimilar market share averages 35% for mature products, while European markets reach 75-85%. The difference comes down to reimbursement policy. Europe uses reference pricing, where all drugs in a class get the same payment. The U.S. system still ties biosimilar reimbursement to the higher-priced reference product, reducing financial incentive to switch.
Can a pharmacy substitute a biosimilar for the reference product like a generic?
No. Unlike generics, biosimilars are not automatically interchangeable. Only biosimilars designated as "interchangeable" by the FDA can be substituted without the prescriber’s permission-and as of 2025, only a handful have received that status. Most require a new prescription if switching.
Final Thoughts
The current biosimilar billing system was designed to encourage competition. But it’s built on a flawed assumption: that providers will choose cheaper drugs if they’re available. In reality, when the profit margin barely changes, they don’t. The fix isn’t more paperwork or more codes-it’s a payment structure that actually rewards savings. Until then, the gap between U.S. and European adoption will keep growing. And patients will keep paying more than they should.