Primary Sclerosing Cholangitis, or PSC, isn’t something most people hear about until it hits close to home. It’s a rare, slow-burning disease that attacks the bile ducts-tiny tubes that carry digestive fluid from the liver to the intestines. Over time, these ducts get scarred, narrowed, and blocked. Bile backs up in the liver, poisoning it. The damage builds silently. By the time symptoms show up, the disease is often far along.
What Happens Inside the Body?
In PSC, the immune system turns against the bile ducts. No one knows exactly why. But we do know it’s not caused by alcohol, drugs, or poor diet. It’s autoimmune: your own body’s defenses start attacking the lining of your bile ducts. This triggers chronic inflammation. Scar tissue forms. The ducts stiffen, shrink, and eventually close off.
Think of it like rust clogging a pipe. At first, the flow slows. Then, it stops. Bile can’t reach the gut to help digest fats. Instead, it pools in the liver, causing damage. Over years, this leads to cirrhosis-hard, fibrous tissue replacing healthy liver cells. Eventually, the liver fails.
The scarring doesn’t just happen inside the liver. It affects ducts both inside (intrahepatic) and outside (extrahepatic) the organ. On imaging tests like MRCP, doctors see a "beaded" pattern-narrow spots next to wider ones-as if someone had pinched the ducts at random intervals. Normal bile ducts are 3 to 8 millimeters wide. In PSC, they often shrink to less than 1.5 mm.
Who Gets PSC-and Why?
PSC doesn’t pick randomly. It favors men. About two out of every three patients are male. Most are diagnosed between 30 and 50, with the average age at diagnosis being 40. It’s more common in Northern Europe. In Sweden, about 6 in 100,000 people have it. In the U.S., roughly 25,000 people are living with PSC.
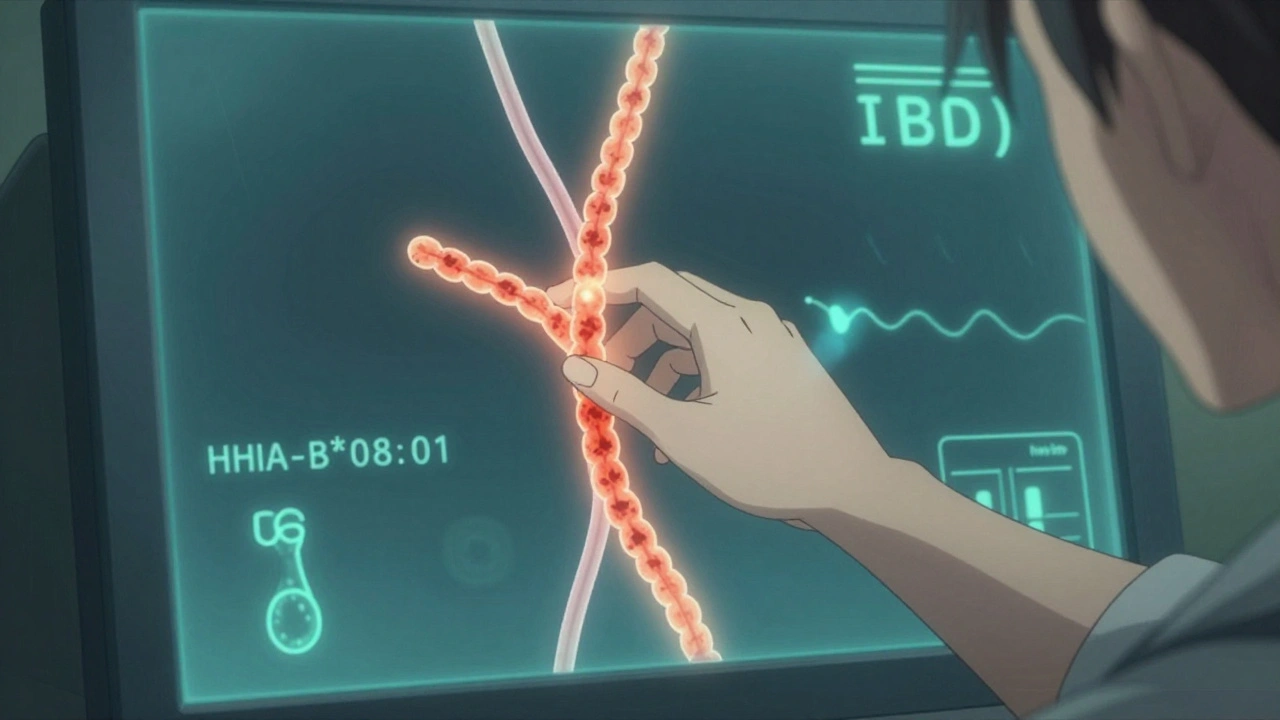
Genetics play a big role. People with a specific gene variant-HLA-B*08:01-are over twice as likely to develop PSC. But genes alone don’t cause it. Something in the environment triggers it. And that something? Likely the gut.
Up to 80% of PSC patients also have inflammatory bowel disease, especially ulcerative colitis. The gut and liver are connected by a highway called the gut-liver axis. When the gut lining is inflamed, bacteria and their waste products leak into the bloodstream and reach the liver. In people with the right genetic setup, this sparks an immune attack on the bile ducts.
Unlike Primary Biliary Cholangitis (PBC), which mostly affects women and shows clear antibodies in blood tests, PSC has no reliable blood marker. Only 20-50% of patients test positive for p-ANCA, and even that’s not specific. That’s why diagnosis often takes years.
How Is It Diagnosed?
There’s no single blood test for PSC. Liver enzymes like ALP and GGT often rise early, but they can also spike from other causes. So doctors look for the pattern: elevated enzymes + symptoms + imaging findings.
The gold standard is MRCP-a non-invasive MRI scan that creates detailed pictures of the bile ducts. It shows the telltale beading. If MRCP is unclear, doctors may use ERCP, which involves threading a scope into the bile ducts. But ERCP carries risks, so it’s used only when needed.
Biopsies are rarely used to diagnose PSC because the scarring is patchy. You might miss it. Imaging is more reliable.
Many patients wait 2 to 5 years before getting a correct diagnosis. Fatigue, itching, and vague abdominal discomfort are dismissed as stress, aging, or IBS. By the time PSC is confirmed, the liver may already be significantly damaged.
What Are the Symptoms?
Early on, many people feel fine. No jaundice. No pain. Just tiredness-deep, unrelenting fatigue that doesn’t go away with sleep. Then comes the itching. Not just a skin rash. Patients describe it as if the itch is coming from inside their bones. It gets worse at night. Some say it’s worse than pain.
Other signs include:
- Yellowing of skin and eyes (jaundice)
- Dark urine and pale stools
- Abdominal pain, especially in the upper right
- Unexplained weight loss
- Fever and chills (sign of infection in the ducts)
One of the most frustrating parts? Symptoms don’t always match how far the disease has progressed. Someone with mild scarring might have terrible itching. Another with advanced cirrhosis might feel fine. That’s why regular monitoring is critical.
There’s No Cure. But There Are Ways to Manage It.
For now, liver transplant is the only cure. But it’s not the first step. Most people live for years without needing one. The goal is to slow damage, manage symptoms, and catch complications early.
For years, doctors prescribed high-dose ursodeoxycholic acid (UDCA) to improve bile flow. But large studies show it doesn’t improve survival. At high doses (28-30 mg/kg/day), it may even increase the risk of serious problems. The European Association for the Study of the Liver now advises against routine use.
So what works?
Managing Itching
Itching is the worst symptom for most patients. First-line treatments include:
- Rifampicin (150-300 mg daily): Helps about half of patients.
- Naltrexone (50 mg daily): Blocks opioid receptors involved in itch signaling.
- Colesevelam (1.89-3.78 g daily): Binds bile acids in the gut to reduce their reabsorption.
Some patients need to try three or four options before finding relief. It’s trial and error-and exhausting.
Monitoring for Cancer
PSC raises your risk of cholangiocarcinoma-bile duct cancer. The annual risk is 1.5%. That may sound low, but over 10 years, it adds up. That’s why annual MRCP scans and tumor marker tests (like CA 19-9) are standard.
Also, if you have ulcerative colitis, you need a colonoscopy every 1-2 years. Your risk of colorectal cancer is 10-15% over your lifetime. Surveillance saves lives.
Preventing Vitamin Deficiencies
When bile can’t reach the gut, your body can’t absorb fat-soluble vitamins: A, D, E, and K. Low vitamin D leads to bone loss. Low vitamin K raises bleeding risk. Quarterly blood tests check these levels. Supplements are often needed-sometimes in high doses.
What’s on the Horizon?
There’s real hope on the horizon. Dozens of drugs are in clinical trials. The most promising target is the FXR receptor, which regulates bile acid production.
Obeticholic acid, tested in the REVERSE trial, lowered liver enzymes by 32% after 18 months. But it caused bad itching and cholesterol spikes, so the FDA hasn’t approved it yet.
Cilofexor, a non-steroidal FXR agonist, showed a 41% drop in ALP in phase 2 trials. It’s now in phase 3. Another drug, norUDCA, is being tested for its ability to protect bile duct cells.
These aren’t cures. But they could slow progression enough to delay transplant. Some experts predict we’ll have at least two approved disease-modifying drugs within five years.
Life With PSC
Living with PSC means learning to live with uncertainty. You might feel fine one month and crash the next. Fatigue can cancel plans. Itching can ruin sleep. The emotional toll is heavy.
But patients who get care at specialized PSC centers report much better outcomes. They get coordinated care-gastroenterologists, hepatologists, nutritionists, and mental health support all in one place. One survey found 85% of patients at these centers felt their symptoms were better controlled than those treated in general clinics.
Support communities like PSC Partners Seeking a Cure help too. Patients share tips, vent frustrations, and celebrate small wins. One Reddit user wrote: "The itching feels like it’s coming from my bones." That’s the kind of truth you only hear from someone who’s lived it.
Transplant remains the endgame. But survival after transplant is excellent-over 80% at five years. Many patients return to full, active lives. The key? Catching the disease early, managing it well, and staying connected to experts who know PSC inside and out.
What You Should Know Right Now
- PSC is rare, progressive, and currently has no cure-but it’s manageable.
- It’s strongly linked to ulcerative colitis. If you have IBD and unexplained fatigue or itching, ask about PSC.
- There’s no effective drug yet, but new therapies are coming fast.
- Regular monitoring for liver cancer and colon cancer saves lives.
- Specialized care centers make a huge difference in quality of life.
- You’re not alone. Thousands are navigating this-many have found ways to live well.
PSC doesn’t define you. But understanding it? That gives you power. Knowledge turns fear into action. And action-consistent, informed, supported action-is how people with PSC don’t just survive. They thrive.
