Keeping your prescription labels and medication leaflets isn’t just good housekeeping-it’s a safety habit that could save your life. Imagine showing up at the emergency room after a fall, confused and in pain, and the doctors have no idea what medications you’re taking. That’s not a hypothetical. It happens every day. The prescription labels on your pill bottles and the tiny leaflets inside contain critical details: dosage, expiration dates, side effects, drug interactions, and who prescribed it. Lose those, and you risk dangerous mistakes, unnecessary tests, or even hospitalization.
Why This Matters More Than You Think
Every year, around 7,000 people in the U.S. die from medication errors, according to the Institute of Medicine. Many of those errors happen because doctors don’t have a clear picture of what a patient is actually taking. You might think, “I remember my meds,” but when you’re on five, ten, or fifteen different pills, memory fails. Even small changes-like switching from 10mg to 5mg-can be forgotten in the chaos of daily life. The good news? A simple system for storing these documents cuts medication errors by more than half, according to a 2022 study in the Journal of General Internal Medicine. Hospitals that have access to a patient’s complete medication history reduce adverse drug events by 55%. That’s not a small number. That’s life-saving.What’s on a Prescription Label (And Why You Need It)
Federal law requires every prescription label to include specific information. If it’s missing, the pharmacy broke the rules. Here’s what you should see:- Your full name
- Medication name (brand and generic)
- Dosage strength (e.g., 10mg, 500mg)
- How to take it (e.g., “Take one tablet by mouth twice daily”)
- Prescriber’s name and contact info
- Pharmacy name, phone, and address
- Fill date and expiration date
- Refill information
What’s in the Leaflet (And Why You Shouldn’t Throw It Away)
The leaflet inside the bottle is longer and more detailed. It’s not fluff. It’s your safety manual. It includes:- Possible side effects (even rare ones)
- Drug interactions (what not to mix with this pill)
- What to do if you miss a dose
- Storage instructions (some meds need refrigeration)
- Warnings for pregnancy, liver disease, or allergies
- How the drug works in your body
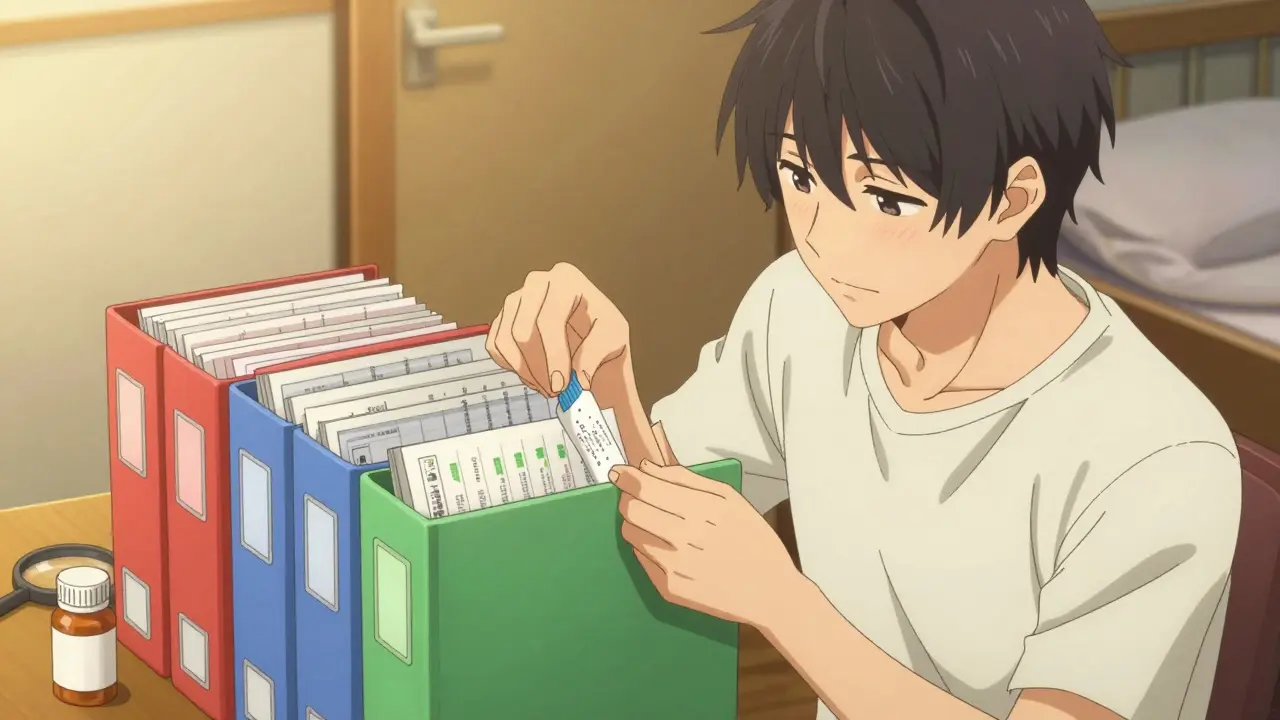
Physical Storage: The Reliable Way
If you’re not tech-savvy, or if you’ve had a bad experience with apps crashing or losing data, physical storage is still the gold standard. Here’s how to do it right:- Get a binder with clear plastic pockets. Look for one labeled “archival quality” or “acid-free.” Regular folders yellow and crumble over time.
- Use color-coded tabs: red for heart meds, blue for antibiotics, green for pain, yellow for mental health. This makes finding things fast.
- Put each label and leaflet together in one pocket. Don’t separate them. You need both.
- Organize alphabetically by medication name. It’s easier than remembering which drug you started first.
- Store the binder in a cool, dry place-like a bedroom drawer, not the bathroom. Heat and humidity ruin paper. The ideal temperature is 68-77°F (20-25°C), same as what most medications need.

Digital Storage: The Smart Backup
Digital isn’t better-it’s different. It’s searchable, backup-ready, and shareable. But it only works if you use it right.- Use a HIPAA-compliant app like MyMedSchedule (version 3.2.1 or later). These apps encrypt your data and don’t sell it.
- Take a clear photo of each label and leaflet with your phone. Don’t just save the pill bottle. Save the full leaflet-even if it’s 10 pages long.
- Label the files clearly: “Lisinopril 10mg - Dr. Patel - 03/2024 - Leaflet.pdf”
- Store copies in two places: your phone and a secure cloud (Google Drive, iCloud, or Dropbox with two-factor enabled).
Combine Both Systems
The best approach? Use both. Keep your current meds in a physical binder. Scan and upload everything older than six months. That way:- You have instant access during emergencies (no phone needed)
- You have a backup if the binder gets damaged by water or fire
- You can email your list to a new doctor in seconds
What Not to Do
Don’t toss old pill bottles just because you’re done with the meds. That’s the #1 mistake people make. One user on PharmacyTechForum lost $1,200 in unnecessary tests because they couldn’t prove they’d been on the same dose for 10 years. Don’t store everything in a shoebox. Moisture, bugs, and time will destroy it. Don’t rely on memory. Don’t assume your doctor has your full record-most EHR systems only keep 7-10 years of data.How Often to Update
Set a reminder: every 3 months, spend 10 minutes reviewing your binder or app. Do this:- Remove expired meds (and dispose of them safely)
- Add new prescriptions
- Update dosage changes
- Check for new leaflets (some meds get updated warnings)

What If You’re Over 65 or Have Many Meds?
If you take five or more medications daily (45% of adults over 65 do), this system isn’t optional-it’s essential. Dr. Jerry H. Gurwitz, a leading geriatrician, says keeping organized records reduces dangerous drug combinations by 32% in older adults. Consider asking your pharmacist for a printed summary. Many pharmacies now offer a “medication reconciliation sheet” for free. Keep that with your binder.Privacy and Security
Digital storage is convenient, but it’s not risk-free. Prescription data is 40 times more valuable than credit card info on the black market, according to IBM’s 2023 report. Only use apps that are HIPAA-compliant. Avoid free apps that ask for your email or phone number to “personalize your experience.” If it sounds too easy, it’s probably selling your data. For physical storage, keep your binder locked or in a secure drawer. Don’t leave it on your kitchen counter.Where to Get Help
If you’re overwhelmed:- Call the CDC Medication Safety Helpline: 1-800-232-0233. They’ll mail you a free template for organizing your records.
- Download the free guide “Your Medication Record: A Patient’s Guide” from the Institute for Safe Medication Practices. It’s been downloaded over 37,000 times.
- Ask your pharmacist to help you set up your first binder. Most are happy to do it.
Final Thought: It’s Not About Perfection
You don’t need a fancy binder or a perfect app. You just need to start. Even keeping a shoebox with labels and leaflets in a dry closet is better than nothing. The goal isn’t to be organized for Instagram. It’s to be prepared for a moment when your life depends on it.One day, someone will ask you: “What are you taking?” Don’t let them guess. Don’t let them wait. Have the answer ready.
How long should I keep prescription labels and leaflets?
Keep them for at least 10 years, especially for chronic conditions like high blood pressure, diabetes, or mental health meds. Some states, like California, legally require 10-year retention. Even if you’re not required to, keeping them longer helps if you switch doctors, move, or need to prove past use for insurance or disability claims.
Can I just take pictures of my labels instead of keeping the paper?
Yes-but only if you back them up. A photo on your phone can be lost if the phone dies, breaks, or gets stolen. Use a HIPAA-compliant app that stores copies in the cloud, or save them to two separate cloud accounts (like Google Drive and iCloud). Always keep the original paper labels for your current meds in case the app fails during an emergency.
What if I can’t read the tiny print on the leaflet?
The FDA requires prescription labels to use 18-point bold font for key info, which is readable for most people. But leaflets are often small print. Use a phone magnifier app or a simple handheld magnifying glass. You can also call your pharmacy and ask them to email or mail you a larger-print version. Most pharmacies will do it for free.
Should I keep labels for over-the-counter meds too?
Yes, especially if you take them regularly. Pain relievers, sleep aids, antacids, and supplements can interact with prescription drugs. A 2023 Consumer Reports survey found that 41% of medication errors involved OTC drugs. Keep a separate section in your binder for these.
What if I don’t have space for a binder?
Start small. Use a manila envelope labeled “Current Meds” and keep it in your purse, wallet, or nightstand. Add new labels as you get them. Once you have 10-15, upgrade to a binder. The goal isn’t perfection-it’s consistency. Even a single envelope with your top three meds is better than nothing.
How do I dispose of old labels safely?
Shred them or tear them into pieces so your name and prescription info can’t be read. Don’t just throw them in the trash. Identity thieves can use that info to fake prescriptions. If you’re unsure, take old bottles to a pharmacy with a drug disposal bin. Most pharmacies offer this for free.