When your doctor switches your prescription from a brand-name drug to a generic version, it’s not just a paperwork change-it’s a moment that can affect how you feel every day. You might not notice anything different. Or you might feel off, confused, or even scared. That’s normal. And the key to getting through it without stress? Communication with your pharmacy.
Why Generics Are Replacing Brand Names
Generic drugs aren’t cheaper because they’re worse. They’re cheaper because they don’t need to pay for the original research, marketing, or patent protection. The FDA requires generics to have the same active ingredient, strength, and dosage form as the brand-name version. They must also deliver the same amount of medicine into your bloodstream at the same speed-within a strict 80% to 125% range. That’s not a guess. It’s science. In 2023, about 90% of all prescriptions filled in the U.S. were generics. They saved patients and insurers $373 billion that year. For many people, switching means saving $20, $50, or even $200 a month. If you’re on Medicare Part D, that’s an average of $265 saved per medication annually. But here’s the thing: even when the science says they’re the same, your body might react differently. That’s why talking to your pharmacist isn’t optional-it’s essential.What Changes When You Switch?
Generics look different. They might be a different color, shape, or size. They might have a different marking on the pill. That’s because inactive ingredients-like dyes, fillers, or coatings-are not required to match the brand name. These don’t affect how the drug works, but they can affect how your body absorbs it… especially if you’re taking a medicine with a narrow therapeutic index. Drugs like levothyroxine (for thyroid), warfarin (a blood thinner), or certain epilepsy meds like phenytoin or levetiracetam fall into this category. Small changes in how much of the drug reaches your bloodstream can mean the difference between control and crisis. A 2021 JAMA study found that 9.4% of patients on generic antiepileptic drugs had a seizure after switching, compared to 5.3% who stayed on brand. That’s not a huge number-but it’s enough to matter. If you’ve ever looked at your new pill and said, “This isn’t the one I’ve been taking,” you’re not alone. In a 2022 survey, 37% of patients hesitated to take a generic just because it looked different. That hesitation can lead to missed doses-and that’s riskier than the switch itself.When to Start Talking to Your Pharmacy
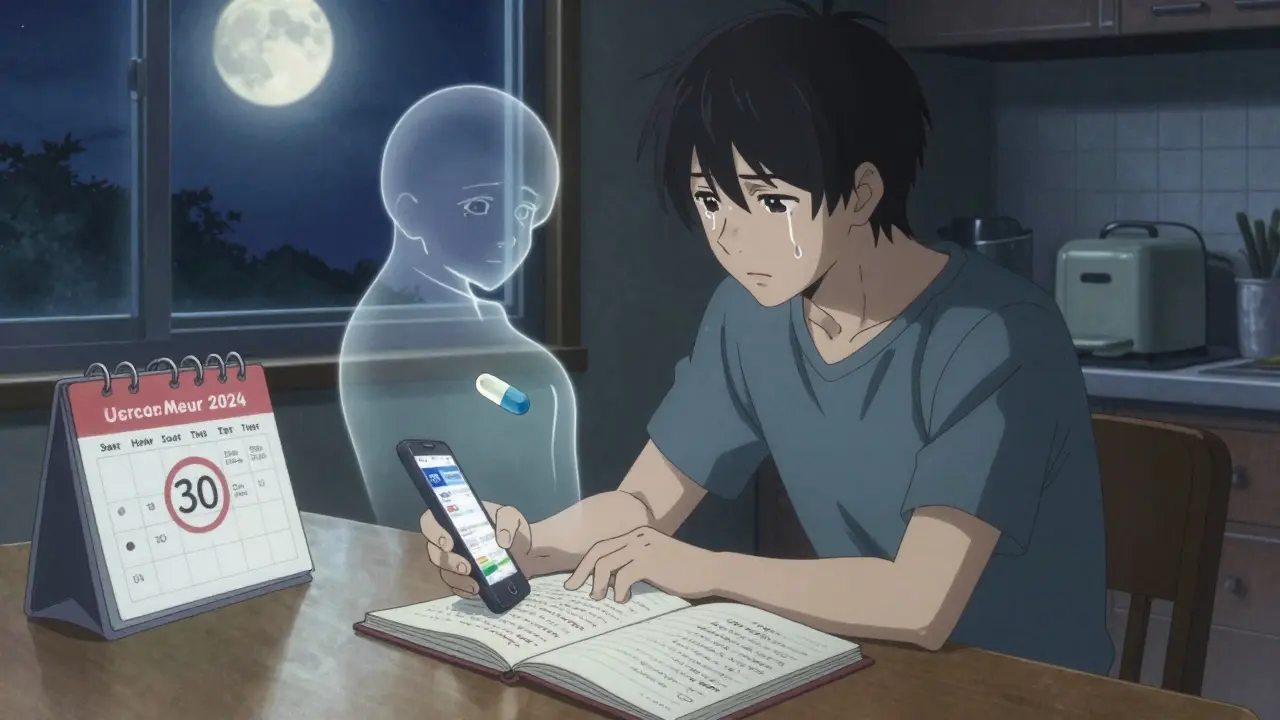
Don’t wait until your last bottle is empty. Start the conversation at least 30 days before your brand-name drug runs out. That gives your pharmacy time to check your insurance, confirm coverage, and order the generic if needed. Here’s what to ask:- “Is this generic approved by the FDA?”
- “Will this work the same way as my old pill?”
- “Are there any known issues with this specific generic manufacturer?”
- “Can I keep the brand if I need to?”
- “Will my insurance cover the brand if the generic doesn’t work?”
What Your Pharmacist Should Do
Good pharmacies don’t just hand you a new bottle. They take responsibility. When a generic switch happens, your pharmacist should:- Check your full medication list for interactions
- Confirm the dose hasn’t changed
- Explain why the pill looks different
- Ask if you’ve had side effects before
- Document your concerns in your file
- Offer to call your doctor if you report problems

What to Do If You Feel Different
If you start feeling worse after switching-more fatigue, more anxiety, more seizures, more dizziness-don’t ignore it. Don’t assume it’s “all in your head.” Write down:- When you started the new pill
- What symptoms you’re having
- How severe they are
- When they started and if they’ve gotten better or worse
Insurance, Transfers, and the New Rules
In August 2023, the DEA changed the rules. Before, if you wanted to switch pharmacies while on a controlled substance-like a painkiller or ADHD med-you had to go back to your doctor to reissue the prescription. Now, you can ask your current pharmacy to transfer the prescription electronically. No doctor visit needed. That’s huge. It means if your old pharmacy runs out of stock or your insurance changes, you can switch without delay. Just walk into a new pharmacy with your ID and the name of your medication. They can pull your prescription directly. Also, Medicare Part D plans must give you 90 days to continue your brand-name drug if you’re new to the plan and it’s not on their formulary. Use that time wisely. Talk to your pharmacist. Try the generic. If it doesn’t work, they can help you appeal.What You Can Do Today
You don’t need to wait for a switch to happen. Here’s how to be ready:- Keep an updated list of every medication you take-name, dose, why you take it, and how often. Keep it in your phone and your wallet.
- Ask your pharmacist every time you pick up a prescription: “Is this the same as last time?”
- If you see a change in pill appearance, ask why.
- Ask if your drug has a narrow therapeutic index. If yes, be extra cautious.
- Sign up for medication synchronization so you never run out.
- Know your insurance’s formulary. Check if generics are preferred. Ask your pharmacy to show you.
When to Push Back
You have rights. If your insurance forces a switch and you’ve had problems before, you can request a formulary exception. Your doctor can write a letter saying the generic won’t work for you. Your pharmacist can help you file it. Many people give up here. Don’t. You’re not being difficult-you’re being smart. For drugs like levothyroxine, the FDA even recommends sticking with the same manufacturer if possible. Why? Because even though all generics meet the same standard, different manufacturers can have slight variations in how they release the drug. If you’ve been stable on one, don’t switch again unless you have to.It’s Not About Trusting the System. It’s About Trusting Yourself.
The system is designed to save money. That’s good. But your health isn’t a line item. If you feel different after a switch, that’s data. That’s real. Your pharmacist is your ally-not a gatekeeper. They’ve seen this before. They know which generics have caused issues for others. They can help you avoid pitfalls. You don’t need to be an expert. You just need to speak up.Are generic drugs really as safe as brand-name drugs?
Yes. The FDA requires generics to meet the same strict standards for safety, strength, quality, and performance as brand-name drugs. They must deliver the same active ingredient in the same way and within the same time frame. Over 90% of prescriptions in the U.S. are filled with generics, and they’ve been used safely for decades. But while they’re equally effective for most people, some individuals-especially those on narrow therapeutic index drugs-may respond differently due to variations in inactive ingredients or manufacturing processes.
Why do generic pills look different from brand-name ones?
Generics can’t copy the exact appearance of brand-name pills because of trademark laws. That means the color, shape, size, or markings might be different. But the active ingredient is identical. These visual differences don’t affect how the drug works, but they can cause confusion or anxiety. Always ask your pharmacist to explain any changes in appearance. If you’re used to a certain look, write down the details so you can recognize future changes.
Can I ask to stay on my brand-name drug even if a generic is available?
Yes. If you’ve had a bad reaction to a generic, or if your doctor believes the brand is better for you, you can request a formulary exception. Your pharmacist can help you submit the paperwork. Insurance may require a letter from your doctor explaining why the generic won’t work. Many patients successfully appeal these decisions, especially for drugs like thyroid medication, epilepsy treatments, or blood thinners.
What should I do if I think the generic isn’t working?
Don’t stop taking it. Write down your symptoms-when they started, how bad they are, and what’s changed. Call your pharmacy right away. They can check if the generic is from a different manufacturer, verify your dose, and contact your doctor if needed. In many cases, they can switch you back to the brand or try a different generic. For controlled substances, the DEA now allows pharmacies to transfer prescriptions electronically without a doctor’s visit, so you can switch locations quickly if needed.
Do I need to tell my pharmacist every time I get a new prescription?
Yes. Even if you’ve been going to the same pharmacy for years, always confirm the medication name, dose, and manufacturer each time. Generic manufacturers change. A pill that looked the same last month might be from a different company this month. Your pharmacist needs to know your history to catch potential issues. Bring your updated medication list to every visit. It’s the best way to avoid mistakes.
Are there any medications I should never switch to generic?
There’s no official list, but experts advise extra caution with drugs that have a narrow therapeutic index-meaning small changes in blood levels can cause big effects. These include levothyroxine, warfarin, phenytoin, cyclosporine, and some epilepsy medications like carbamazepine or lamotrigine. If you’ve been stable on a brand for years, discuss with your doctor and pharmacist before switching. Sometimes staying on the same version-brand or generic-is safer than switching back and forth.
Next Steps: What to Do After the Switch
After you start the generic:- Take it exactly as directed for at least two weeks before judging how it feels.
- Track your symptoms in a simple notebook or phone note.
- Set a reminder to check in with your pharmacist in 30 days.
- If you feel better-great. If you feel worse, don’t wait. Call them.
- Ask if the generic manufacturer offers a patient support line. Many do.
