Every year, millions of people stop taking their medicine-not because it doesn’t work, but because they don’t understand what they’re taking. For many, the switch from a brand-name drug to a generic feels like a trick. The pill looks different. The name on the bottle is unfamiliar. The price dropped, but the fear didn’t. Health literacy isn’t just about reading a label. It’s about trusting what you read. And when it comes to generics, that trust is often missing.
What Exactly Is a Generic Medication?
A generic drug is not a copy. It’s not a knockoff. It’s the exact same medicine as the brand-name version, just without the marketing. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the original. That means if your brand-name blood pressure pill has 25mg of lisinopril, so does the generic. The same chemical. The same effect. The same way it works inside your body. The differences? Only in the inactive parts. The color. The shape. The filler. These don’t affect how the drug works. But they’re exactly what cause confusion. A 2023 study found that 63% of people with low health literacy couldn’t identify the active ingredient on a generic label-compared to just 28% on a brand-name label. That’s not a failure of intelligence. It’s a failure of communication.Why Do People Think Generics Don’t Work?
The myth that generics are weaker isn’t just common-it’s deeply rooted. One in every two patients in the U.S. believes generic drugs are less effective than brand-name ones. That’s not based on science. It’s based on appearance. And fear. Think about this: if you’ve been taking a blue, oval pill for years, then your pharmacist hands you a white, round one with a different name, your brain says: “This isn’t the same.” Your body doesn’t know the difference. But your mind does. And that’s where the problem starts. Patients report stopping their meds because:- The pill looks different
- The name on the bottle doesn’t match what their doctor said
- They think the lower price means lower quality
- They don’t understand what “bioequivalent” means
Who Gets Left Behind?
This isn’t a problem for everyone equally. The people most affected are the ones who already face barriers: older adults, immigrants, people with low income, those who speak English as a second language, and people with limited education. A 2025 study from NYU found that immigrants and non-native English speakers are over three times more likely to misunderstand generic medication instructions. Why? Because most patient materials are written at a 10th-grade reading level-even though nearly half of U.S. adults read at or below an 8th-grade level. Imagine being handed a prescription for a generic antidepressant. The label says “Sertraline Hydrochloride.” You’ve never heard that word. Your doctor said “Zoloft.” You don’t know if it’s the same. You don’t know who to ask. So you don’t take it. That’s not negligence. That’s a system failure.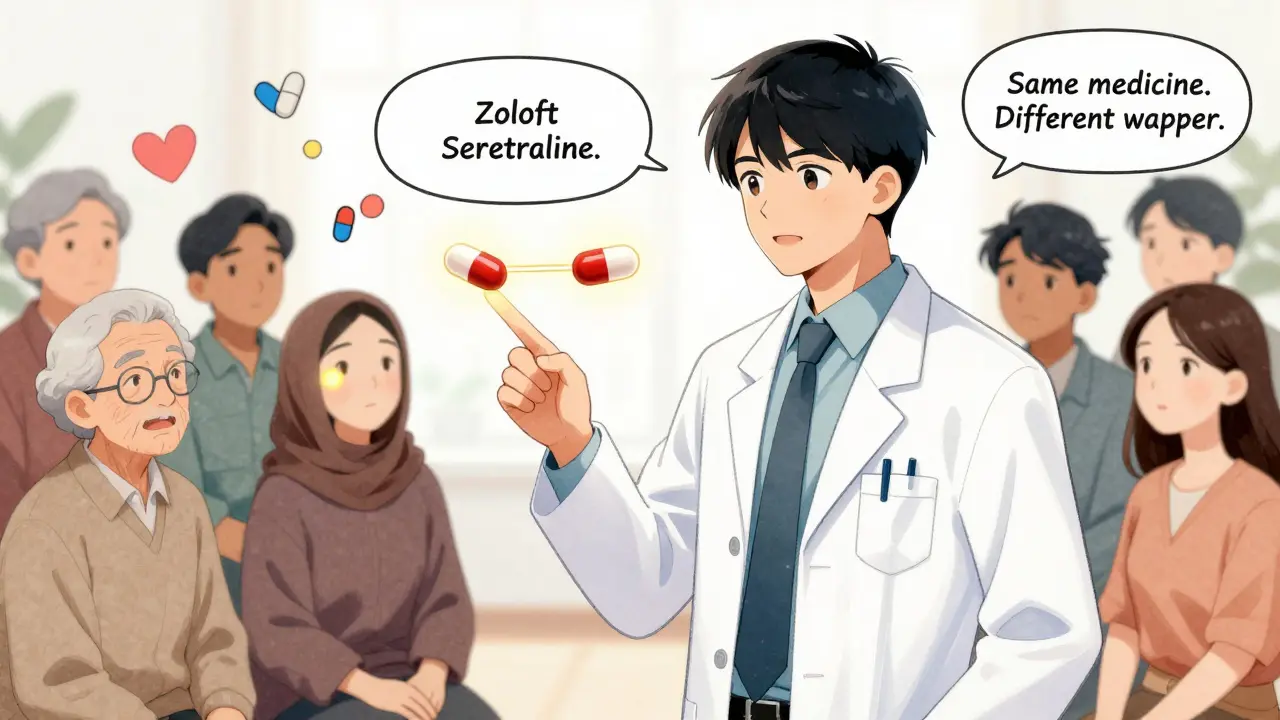
How Pharmacists Can Close the Gap
Pharmacists are on the front lines. But they’re often rushed. On average, they spend just over four minutes explaining a generic substitution. For patients with low health literacy? That jumps to nearly ten minutes. And even then, many don’t know how to explain it clearly. The most effective tool? The Teach-Back method. Instead of asking, “Do you understand?”-which most people say yes to, just to be polite-pharmacists ask: “Can you tell me in your own words what this medicine is for and why you’re taking it?” One CVS patient said: “My pharmacist showed me a picture of the brand pill and the generic side by side. He said, ‘Same medicine. Different wrapper. Just like your favorite soda comes in different bottles.’ That made sense.” That’s the kind of clarity that works. Visuals. Analogies. Plain language. No jargon. No “bioequivalence.” Just: “This works the same way. It’s cheaper. And it’s safe.”What Health Systems Are Doing Right
Some clinics and pharmacies are starting to fix this. A pilot program in Atlanta used simple picture-based guides to show patients how to match generic pills to their brand names. Within six months, medication errors dropped by 29%. Adherence went up by 22%. In 2023, the FDA launched a national “Generics Awareness Campaign” with free, plain-language handouts for pharmacies. The CDC now includes “understanding generic alternatives” as a key goal in its Health Literacy Action Plan. And starting in 2024, Medicare Part D plans must assess patients’ health literacy before dispensing high-cost medications. But most health systems still don’t have a plan. Only 38% of U.S. healthcare organizations have any formal program to help patients understand generics. That’s not progress. That’s negligence.
What You Can Do Right Now
If you or someone you care about is on medication:- Ask your pharmacist: “Is this the same as the brand-name version?”
- Ask them to show you a picture of both pills side by side.
- Ask: “What’s the active ingredient?” Write it down.
- Use a pill identifier app (like Medscape or WebMD) to scan your pill and confirm the name.
- If you’re confused, don’t stop taking it. Call your doctor or pharmacist. No question is too simple.
The Bigger Picture: Why This Matters
Generics make up 90% of all prescriptions filled in the U.S. But they cost only 23% of what brand-name drugs do. That’s billions in savings. Billions that go to waste when people don’t take their meds because they think the generic won’t work. The cost isn’t just financial. It’s human. People end up in the ER. Their conditions get worse. Their lives get harder. And all because no one took the time to explain that a different-looking pill can still save their life. Closing this gap isn’t about more brochures. It’s about better conversations. It’s about seeing health literacy not as a patient problem-but as a system problem. And fixing it starts with one simple question: “Do you know what you’re taking?”If the answer is no, then the system failed-not the person.
