Generic Drug Cost Calculator
Calculate Your Savings
Your Savings
Why You Save Money
Generic drugs cost significantly less because they don't include:
- Marketing and advertising expenses
- Patent protection costs
- Extensive brand development
The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and bioavailability as brand-name versions.
According to the FDA, 90% of generic drugs cost less than $10 per month. That's real savings you can see in your wallet.
When you pick up a prescription, you might see two very different-looking pills on the counter. One has a colorful logo and a familiar name. The other is plain, white, and labeled with a long chemical name. You might wonder: Are they really the same? The answer isn’t just yes - it’s backed by science, regulation, and millions of real-world prescriptions.
Same Active Ingredient, Different Look
Generic drugs contain the exact same active ingredient as their brand-name counterparts. That means if you’re taking omeprazole for acid reflux, whether it’s sold as Prilosec or as a generic, the molecule doing the work inside your body is identical. The U.S. Food and Drug Administration (FDA) requires this. No exceptions. No loopholes. The dose, strength, route of administration - all must match.The differences? They’re all on the outside. The shape, color, size, and markings on the pill are changed to avoid trademark infringement. A brand-name drug like Lipitor (atorvastatin) is a blue, diamond-shaped tablet. The generic version? It could be white and oval. That doesn’t mean it’s weaker. It just means it looks different.
Labeling: The Fine Print That Doesn’t Lie
Brand-name drug labels often include marketing language - brand names, slogans, or patient support program details. Generic labels? They’re stripped down. They list the active ingredient by its chemical name (like atorvastatin calcium), not the brand name (Lipitor). But here’s the key: everything that matters for your safety is identical.The FDA mandates that generic drug labels mirror brand-name labels in every clinically relevant way: indications, dosage instructions, contraindications, warnings, and side effects. If the brand-name drug says “May cause dizziness,” so does the generic. If it warns against use in pregnancy, the generic says the same thing. The FDA’s 2021 guidance on labeling ensures there’s no room for misleading differences.
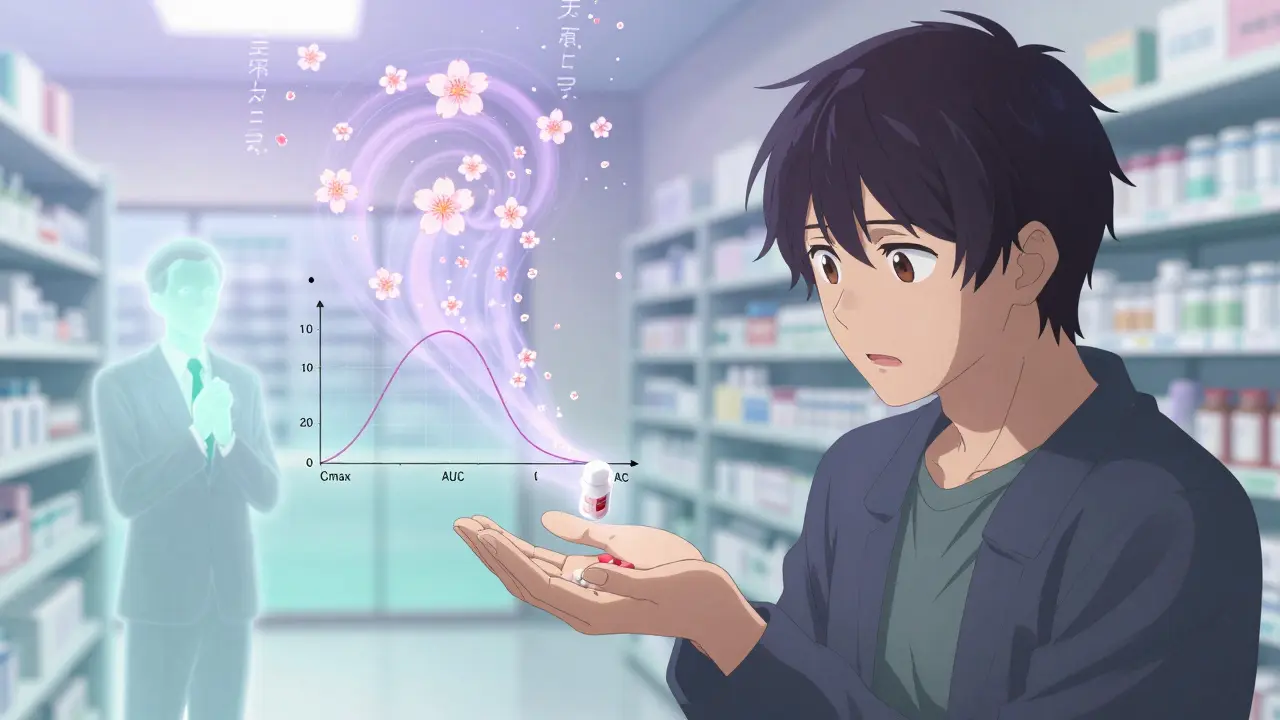
Therapeutic Equivalence: How the FDA Proves They Work the Same
The biggest concern people have is whether generics work as well. The answer comes down to bioequivalence - a strict scientific test. Before a generic is approved, the manufacturer must prove it releases the same amount of active ingredient into your bloodstream at the same rate as the brand-name drug.This is measured using two key metrics: Cmax (the highest concentration in your blood) and AUC (the total exposure over time). The FDA requires these numbers to fall within 80% to 125% of the brand-name drug’s values. That’s not a wide range - it’s tighter than the natural variation you’d see between two different batches of the same brand-name drug.
Dr. Ameet Nagpal, a pharmacy expert at Northwestern Medicine, put it plainly: “The 20% variability allowed in bioequivalence studies is actually stricter than the natural variation within brand-name drug batches.” In other words, the generic you get today might be more consistent than the brand-name version you got last month.
Cost: The Real Difference
The biggest gap between generic and brand-name drugs isn’t in effectiveness - it’s in price. Generic drugs cost, on average, 80% to 85% less. Take atorvastatin: the brand-name Lipitor cost around $375 per month in early 2023. The generic? At Walmart, it was $4.00 for a 30-day supply. That’s not a typo.From 2007 to 2016, generic drugs saved the U.S. healthcare system $1.67 trillion. In 2023 alone, they saved $313 billion. The FDA reports that 90% of generics cost less than $10 per month. For people on fixed incomes, chronic conditions, or without good insurance, that difference isn’t just savings - it’s access to medicine.
When You Should Be Cautious
Most drugs are safe to switch. But there’s a small group called narrow therapeutic index (NTI) drugs where even tiny changes in blood levels can matter. These include warfarin (a blood thinner), levothyroxine (for thyroid issues), and phenytoin (for seizures). For these, the FDA recommends close monitoring when switching between brands or even between different generic manufacturers.A 2021 study in JAMA Internal Medicine tracked over 2 million patients on cardiovascular drugs and found no difference in outcomes between generics and brand-name versions. But for NTI drugs, doctors often stick with one manufacturer - brand or generic - to avoid any potential variability in inactive ingredients that might affect absorption.
What Patients Actually Experience
Real-world feedback tells a clear story. On Drugs.com, generic atorvastatin has an average rating of 6.6 out of 10 from nearly 2,000 reviews. Lipitor, the brand, scores 6.3. That’s not a gap - it’s nearly identical. Sixty-two percent of users reported “moderate to significant cost savings” with no loss in effectiveness.But people do notice the pills look different. A University of Michigan study found 12% of patients hesitated when they got a new pill - not because it didn’t work, but because it looked unfamiliar. Some thought they’d been given the wrong medicine. Pharmacists often get calls like: “This isn’t the same pill!” - and the answer is always: “It’s the same drug. Just a different look.”
How Substitution Works in Practice
In 49 U.S. states, pharmacists can automatically switch your brand-name prescription to a generic unless your doctor writes “Dispense as Written” on the prescription. That’s the law. It’s designed to save money without asking you to do anything extra.Most doctors - 94% according to the American Medical Association - feel confident prescribing generics. They know the science. They’ve seen the data. They’ve watched patients stick to their meds because they can afford them.
What About Complex Drugs?
Not all drugs are easy to copy. Biologics - like insulin, monoclonal antibodies, or EpiPens - are made from living cells, not chemicals. Their complexity makes exact copies impossible. Instead, we get “biosimilars,” which are highly similar but not identical. The FDA has approved fewer of these, and they’re still expensive. But even here, progress is happening. In September 2023, the first generic version of semaglutide (Ozempic) was approved for type 2 diabetes - a major milestone.The FDA’s 2024-2028 plan aims to speed up reviews for complex generics by 20%. In 2022, they approved 79 complex generics - up 22% from the year before. That means more affordable options are coming for conditions like asthma, diabetes, and autoimmune diseases.
What You Should Do
If you’re taking a regular medication - blood pressure pills, statins, antidepressants, antibiotics - there’s no reason not to use the generic. Ask your pharmacist. Ask your doctor. Check the FDA’s Orange Book, which lists all approved generics and their therapeutic equivalence ratings. If it’s rated “A,” it’s considered interchangeable.If you’re on a narrow therapeutic index drug, talk to your provider before switching. Keep track of how you feel. Get lab tests done if needed. But don’t assume the generic won’t work - assume it will, unless your doctor says otherwise.
And if you’re worried about the color or shape of your pill? Call your pharmacy. Ask them to explain the change. Most will show you the FDA’s official documentation. You’re not being paranoid. You’re being informed.
Bottom Line
Generic drugs aren’t cheaper because they’re worse. They’re cheaper because they don’t carry the cost of marketing, advertising, and patent protection. The active ingredient, the dose, the safety profile - all are the same. The FDA doesn’t approve a generic unless it works just like the brand.For most people, choosing a generic isn’t a compromise - it’s a smart, safe, and proven way to save money without losing health.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Studies involving millions of patients show no meaningful difference in effectiveness for most drugs.
Why do generic pills look different from brand-name ones?
U.S. trademark laws require generic drugs to look different from brand-name versions. This means different colors, shapes, sizes, or markings. These changes are purely cosmetic and have no effect on how the drug works. The active ingredient and its performance in your body remain identical.
Can I trust generics if they cost so much less?
Absolutely. Generic drugs cost less because manufacturers don’t spend money on advertising, branding, or patent recovery. The FDA holds them to the same manufacturing standards as brand-name drugs - same facilities, same inspections, same quality controls. The savings come from competition, not lower quality.
Are there any drugs I shouldn’t switch to generic?
For most drugs, switching is safe. But for narrow therapeutic index (NTI) drugs - like warfarin, levothyroxine, or phenytoin - small changes in blood levels can matter. Your doctor may recommend sticking with one brand or generic manufacturer to avoid potential fluctuations. Always discuss this with your provider before switching.
How do I know if a generic is approved by the FDA?
Check the FDA’s Orange Book, which lists all approved generic drugs and their therapeutic equivalence ratings. If a generic is rated "A," it means it’s considered interchangeable with the brand-name drug. You can also ask your pharmacist - they have access to this information and can confirm approval status.
Why do some people say generics don’t work for them?
Sometimes, it’s confusion over pill appearance. Other times, people notice side effects after switching - but those are often due to changes in inactive ingredients, not the active drug. Rarely, a person might be sensitive to a filler in one generic version but not another. If you feel different after switching, talk to your doctor or pharmacist. It’s rarely the generic itself - more often, it’s an adjustment period or an unrelated issue.
Can pharmacists switch my prescription to a generic without asking me?
In 49 U.S. states, yes - unless your doctor writes "Dispense as Written" on the prescription. Pharmacists are allowed to substitute generic versions automatically because they’re proven to be safe and effective. This is a standard practice designed to lower costs. You can always ask for the brand-name version, but you may pay more.
Do generic drugs take longer to work?
No. Bioequivalence testing ensures generics reach the same peak concentration in your blood at the same time as the brand-name drug. If the brand works in 30 minutes, so does the generic. If the brand is extended-release, the generic must match that release pattern exactly. There’s no delay in onset or duration.