Garlic Supplement & Anticoagulant Risk Checker
Risk Assessment Tool
When you take garlic supplements for heart health, you might think you're doing something harmless-or even helpful. But if you're also on blood thinners like warfarin, apixaban, or rivaroxaban, you could be putting yourself at serious risk. The problem isn't just theoretical. Real people have bled uncontrollably during routine surgeries, had strokes from spontaneous clots, or ended up in the ER with nosebleeds that wouldn't stop-all because they didn't know garlic supplements can act like a hidden second dose of their blood thinner.
How Garlic Interferes With Blood Clotting
Garlic isn't just a flavoring for pasta. The active compound in garlic supplements, called ajoene, directly blocks platelets from sticking together. Platelets are the tiny cells in your blood that rush to seal cuts and prevent bleeding. When ajoene binds to platelets, it stops them from activating, which sounds good if you're trying to prevent clots-but dangerous if you're already on a blood thinner.
Studies show that even standard doses of garlic supplements (600-1,200 mg daily) can reduce platelet function by 20-40%. That’s comparable to low-dose aspirin. But unlike aspirin, which is monitored by doctors, garlic supplements aren't regulated for consistency. One brand might have 0.1 mg of ajoene per capsule; another might have 1.0 mg. You never know what you're really getting.
The effect doesn’t fade quickly either. Because ajoene permanently disables platelets, your body has to make new ones. That takes 7-10 days. So if you take garlic supplements on Monday, your blood is still thin on Friday. And if you’re on warfarin? The risk multiplies.
What Happens When Garlic Meets Blood Thinners
Anticoagulants work differently than antiplatelet drugs. Warfarin slows down clotting factors in your liver. DOACs like apixaban block specific enzymes. Garlic doesn’t interfere with those mechanisms directly-but it adds another layer of thinning on top.
Case reports are alarming. One man in his 70s developed a spinal hematoma after taking 2,400 mg of garlic daily. He didn’t have trauma, no fall, no injury. Just garlic and time. Another patient had a colon surgery and bled so badly the surgeons had to switch from minimally invasive to open surgery. Both patients swore they didn’t think garlic was a "medicine."
Lab tests confirm this. Patients on warfarin who took garlic supplements saw their INR jump by 1.0 to 2.5 points. That’s not a small change. INR above 4.0 is considered dangerous-it means your blood takes four times longer to clot than normal. At that level, even a minor bump can lead to internal bleeding.
And it’s not just warfarin. People on apixaban, dabigatran, and rivaroxaban have reported spontaneous nosebleeds, gum bleeding, and bruising that spreads without cause. One Reddit user described nosebleeds lasting over 30 minutes after combining garlic with apixaban. They needed emergency treatment.
Who’s Most at Risk?
You don’t have to be elderly or sick to be in danger. The biggest group at risk? Adults over 65. According to the National Health Interview Survey in 2022, nearly one in five seniors take garlic supplements. And over 22% of them are also on blood thinners. That’s over 3 million Americans quietly mixing two risky substances.
It’s worse if you’re scheduled for surgery-any surgery. Dental work, knee replacements, even colonoscopies can trigger bleeding if garlic is still in your system. A 2017 study found that 68% of patients continued taking garlic supplements within seven days of surgery, even after being asked about herbal use. Why? Because they didn’t think it counted.
Some procedures are especially dangerous. Neurosurgery? A single bleed in the brain can be fatal. Prostate surgery? One case report described four hours of uncontrolled bleeding after a routine procedure. Dental extractions? Even aspirin is often stopped before these, and garlic is stronger.
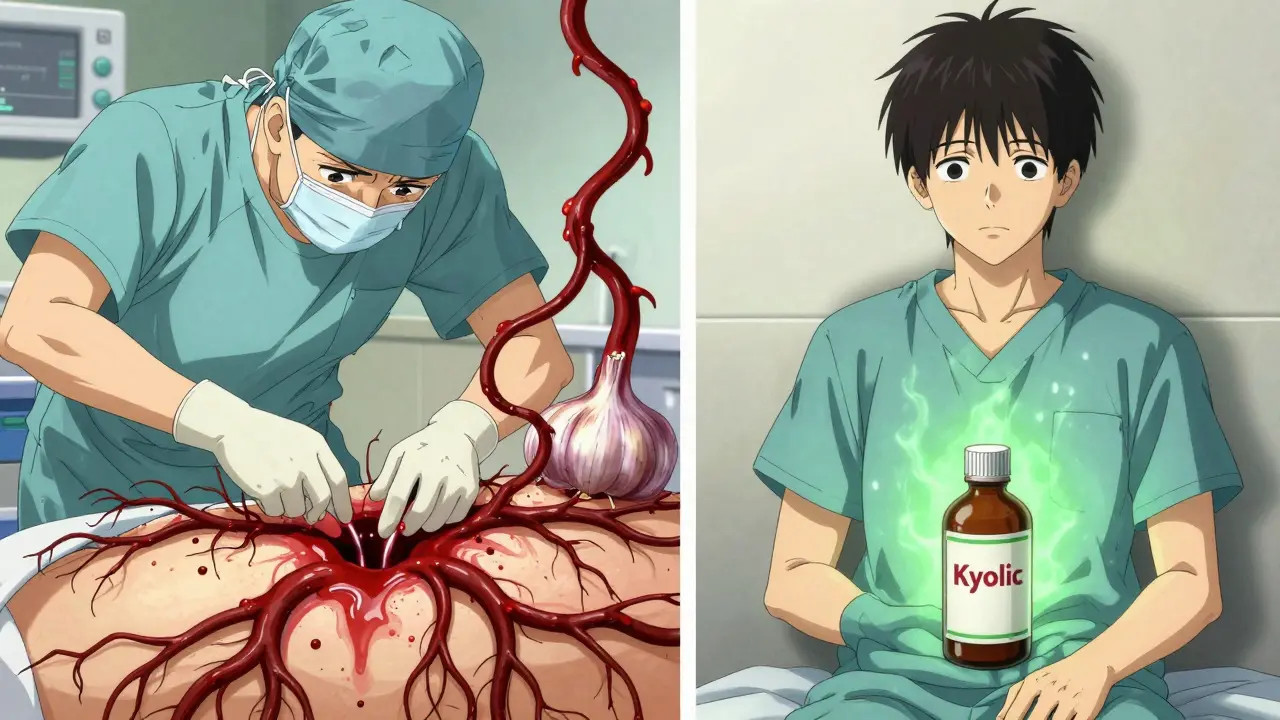
Not All Garlic Supplements Are the Same
Here’s the twist: not every garlic product has the same risk. The type of supplement matters more than you think.
- Oil macerates (garlic soaked in oil) have the highest ajoene-up to 1.0 mg per gram. Highest risk.
- Dried powder supplements (the most common kind) contain 0.1-0.3 mg per gram. Still risky.
- Aged garlic extract (like Kyolic) has almost no ajoene. Studies show it causes little to no platelet inhibition. This is the safest option-if you must take garlic.
Most labels don’t tell you which type you’re getting. They just say "garlic supplement." That’s a problem. A 2019 FDA warning pointed out that potency varies up to 15-fold between brands. You could be taking a dangerous dose without knowing it.
What the Experts Say
Dr. Pieter Cohen from Harvard says garlic supplements can "increase the levels and effects of some medications for heart health, such as blood thinners." The American Society of Anesthesiologists classifies garlic as a "high-risk herbal product" and recommends stopping it 14 days before surgery. The European Society of Anaesthesiology says seven days is enough-but they still say stop it.
The American Heart Association warns: "Garlic supplements should be used with extreme caution in patients taking anticoagulants." Why? Because there are documented cases of life-threatening bleeding. Not just theory. Real people. Real hospitals.
Even skeptics agree on one thing: the lack of labeling is dangerous. A 2022 audit found only 37% of garlic supplement makers even reference the NIH’s LiverTox database, which tracks drug interactions. Most don’t. So you’re flying blind.

What You Should Do
If you’re on a blood thinner and taking garlic supplements:
- Stop taking them immediately. Don’t wait for surgery. If you’re bleeding more than usual-nose, gums, bruises-that’s a sign.
- Switch to aged garlic extract if you want heart benefits. It doesn’t thin your blood.
- Tell every doctor, dentist, and pharmacist you see. Say: "I take garlic supplements." Don’t say "I eat garlic." They need to know about pills, oils, and extracts.
- Ask your doctor to check your INR if you’ve been taking garlic recently. A sudden spike could mean trouble.
- Don’t assume "natural" means safe. Garlic supplements aren’t regulated like drugs. They’re sold like food.
And if you’re not on blood thinners? You’re probably fine. But if you’re considering starting garlic supplements for cholesterol or blood pressure, talk to your doctor first. There are safer ways to support heart health.
The Bigger Picture
The garlic supplement market is booming. Sales hit $1.27 billion in 2022. More people are taking them than ever. But awareness hasn’t kept up. A 2022 GoodRx survey found 83% of users didn’t know garlic could interact with blood thinners. Two-thirds never talked to their doctor about it.
That’s not ignorance. It’s a system failure. Labels don’t warn. Pharmacists don’t ask. Doctors don’t always know. And patients? They think garlic is just food.
The FDA is moving toward requiring ajoene labeling on supplements-expected by mid-2024. But until then, you have to be your own advocate. Because if you’re on a blood thinner, garlic isn’t just a supplement. It’s a hidden drug.
Can I eat garlic while on blood thinners?
Yes, eating fresh or cooked garlic in food is generally safe. The problem is concentrated supplements-pills, oils, extracts-that deliver far more active compound than food. You’d need to eat over a full head of garlic daily to match the dose in a single supplement. Cooking reduces potency, so normal dietary use isn’t a concern.
How long before surgery should I stop garlic supplements?
The American Society of Anesthesiologists recommends stopping garlic supplements 14 days before surgery. The European Society of Anaesthesiology says 7 days is sufficient. Since effects can last up to 10 days, erring on the side of caution is best. Always tell your surgeon and anesthesiologist you took garlic-even if you stopped a week ago.
Are there garlic supplements that don’t interact with blood thinners?
Yes. Aged garlic extract (like Kyolic) contains almost no ajoene and has been shown in studies to have minimal effect on platelets. If you need a garlic supplement for heart health while on anticoagulants, aged garlic extract is the only safe choice. Check the label: if it says "aged" or "odorless," it’s likely the safer option.
What are the signs that garlic is affecting my blood thinners?
Watch for unexplained bruising, nosebleeds lasting more than 10 minutes, bleeding gums when brushing, blood in urine or stool, or unusually heavy menstrual flow. If you’re on warfarin, your INR may rise without any change in dose. If you notice any of these, stop the supplement and contact your doctor immediately.
Why don’t supplement labels warn about this?
In the U.S., supplements aren’t required to prove safety before selling. The FDA can only act after harm is reported. Most garlic supplement labels don’t mention drug interactions because manufacturers aren’t forced to. Only 42% comply with basic labeling standards, and even fewer mention anticoagulant risks. That’s why you need to research products yourself and talk to your pharmacist.
What’s Next?
The NIH is funding a major study to measure exactly how different garlic products affect apixaban levels in the blood. Results are expected by late 2024. Until then, the safest path is clear: if you’re on blood thinners, avoid garlic supplements entirely. There’s no benefit worth the risk. And if you’re not on anticoagulants but thinking about starting garlic, ask your doctor first. There are better, safer ways to protect your heart.
