Digoxin-Amiodarone Dose Adjustment Calculator
Dose Adjustment Calculator
This tool helps calculate the safe digoxin dose adjustment when starting amiodarone therapy. Always monitor levels as recommended.
Recommended Digoxin Dose
Based on guidelines from the article: Reduce by 50% for normal kidney function, 33% for impaired function
Critical Monitoring Steps
Check digoxin level 72 hours after starting amiodarone. Monitor for nausea, vision changes, or irregular heartbeat. Continue monitoring for at least 4 weeks.
Important Safety Note
Digoxin toxicity can occur within days. The 2021 JACC: Heart Failure study showed a 35% 30-day mortality rate when digoxin wasn't adjusted vs 8% with reduction. Never wait for symptoms!
When two powerful heart drugs are taken together, the line between treatment and danger can vanish in days. Digoxin and amiodarone are both lifesavers for patients with atrial fibrillation or heart failure - but when used together without careful management, they can trigger fatal toxicity. This isn’t a theoretical risk. It’s a real, well-documented, and often preventable crisis happening in hospitals and clinics right now.
Why This Interaction Is So Dangerous
Digoxin has a razor-thin safety margin. Its therapeutic blood level? Just 0.5 to 0.9 ng/mL. Go above that, and you risk nausea, vomiting, blurry yellow vision, and dangerous heart rhythms. Go much higher, and you could die. Amiodarone, used to control irregular heartbeats, doesn’t just sit quietly alongside digoxin - it actively interferes with how the body clears it. The science behind this is clear: amiodarone blocks a protein called P-glycoprotein, which normally pushes digoxin out of the body. Without this cleanup crew, digoxin builds up. Studies show serum levels can jump by 100% or more within days of starting amiodarone. That’s not a small change - it’s the difference between a safe dose and a lethal one. And it’s not just the drug itself. Amiodarone’s metabolite, desethylamiodarone, sticks around for months after stopping the medication. That means even if you quit amiodarone, the risk doesn’t disappear overnight. This isn’t a short-term problem. It’s a long-term shadow over every patient on digoxin.What Happens When You Don’t Adjust the Dose
In 2021, a study published in JACC: Heart Failure found that when doctors kept digoxin at full dose after starting amiodarone, 35% of heart failure patients died within 30 days. That’s compared to just 8% when the dose was lowered. That’s a 27% absolute increase in death risk - one of the largest mortality differences ever documented from a simple dosing error. Real-world cases are just as alarming. A 72-year-old woman in Boston was admitted to the ICU with a potassium level of 6.8 mEq/L - dangerously high - and a slow, unstable heart rhythm. She had been on digoxin for years. When her doctor started amiodarone for new-onset atrial fibrillation, no one touched her digoxin dose. Within a week, she was fighting for her life. She survived, but only after four days in intensive care. This isn’t rare. A 2022 study across 15 U.S. hospitals found that in community hospitals, nearly 7 out of 10 patients received the wrong digoxin dose when amiodarone was added. Even in academic centers, more than half of cases missed the necessary adjustment.How to Manage This Interaction Correctly
There’s no mystery here. The solution is simple - but only if you act fast.- Reduce digoxin by 50% the day you start amiodarone. Don’t wait for lab results. Don’t assume the patient is fine. Start with half the dose immediately.
- Check digoxin levels 72 hours after starting amiodarone. This isn’t optional. Levels peak around 1 to 2 weeks, but the first big rise shows up in 3 days. Waiting longer puts the patient at risk.
- For patients with kidney problems (creatinine clearance under 50 mL/min), reduce digoxin to 33% of the original dose. Their bodies clear digoxin slower already. Add amiodarone, and the risk spikes even higher.
- Keep monitoring for at least 4 weeks. Even if levels look good after 72 hours, the interaction can deepen over time. Amiodarone doesn’t rush - it lingers.
Why Doctors Still Get This Wrong
You’d think with all the evidence, this would be routine. But it’s not. One reason? Amiodarone’s long half-life makes the interaction feel invisible. A patient might be on digoxin for years without issue. Then, when amiodarone is added, nothing seems to change right away. The patient feels fine. The doctor assumes it’s safe. But toxicity doesn’t hit on day one - it sneaks in over days or weeks. Another reason? Digoxin is old. It’s cheap. It’s been around since the 1930s. Some doctors treat it like a harmless relic, not a precision tool. But digoxin isn’t aspirin. It’s more like insulin - a drug where a tiny mistake can kill. And then there’s the myth that “we’ve always done it this way.” In one case report, a cardiologist admitted, “I’ve seen three digoxin toxicity cases this year - all in elderly patients with kidney disease. I knew the risk. But I didn’t reduce the dose because I didn’t want to under-treat their heart failure.” That’s the trap. You don’t have to choose between safety and efficacy. You just have to dose correctly.What’s Changing in 2026
Guidelines are shifting. The 2024 European Society of Cardiology draft guidelines now recommend avoiding digoxin altogether in patients with atrial fibrillation who might need amiodarone. Beta-blockers and calcium channel blockers are safer alternatives for rate control. But digoxin still has a place - especially in heart failure patients with low blood pressure or those who can’t tolerate other drugs. That’s why the focus isn’t on eliminating digoxin. It’s on using it smarter. New research is coming. The DIG-AMIO trial (NCT05217891), expected to finish in late 2025, is comparing 50% vs. 33% digoxin dose reductions. It may refine current recommendations. But for now, the safest approach remains: reduce by half at the start. Meanwhile, the market is responding. Digoxin prescriptions in the U.S. dropped 18% between 2015 and 2022. That’s not because it’s obsolete - it’s because doctors are finally learning to respect its danger.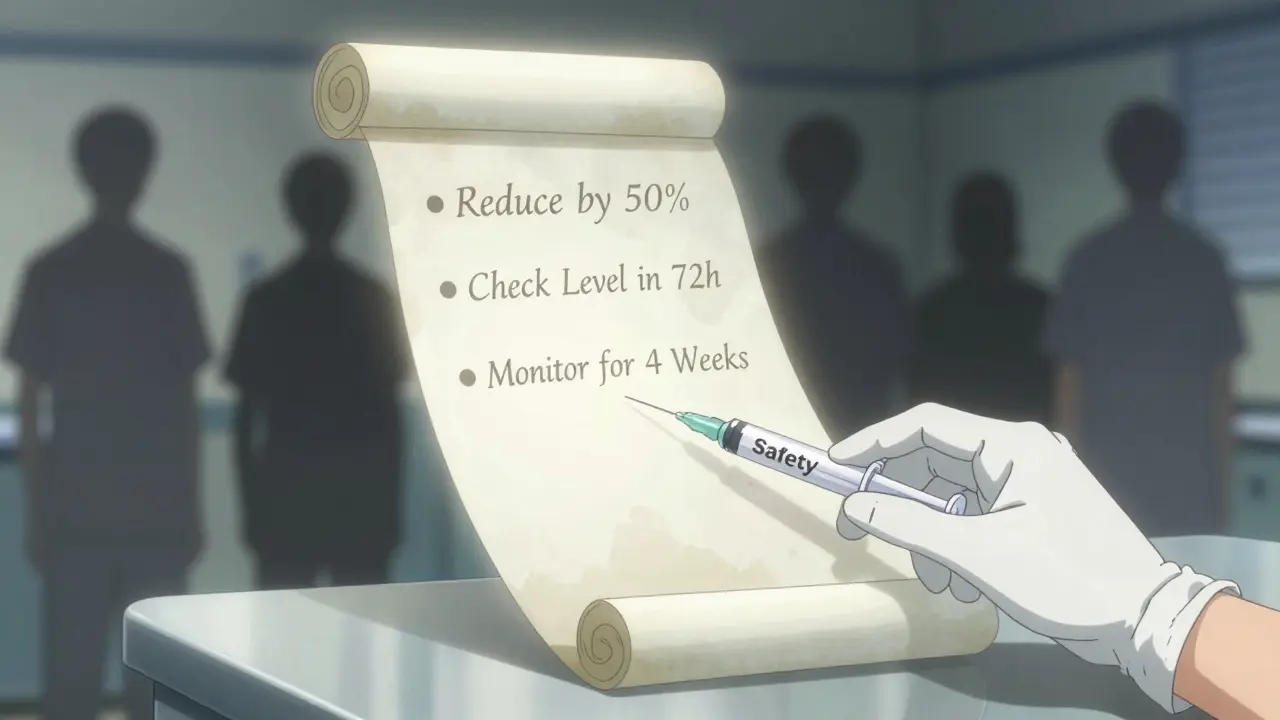
What You Need to Remember
If you’re managing a patient on digoxin and you’re thinking about starting amiodarone - stop. Don’t write the prescription yet. Do this first:- Check the patient’s current digoxin level.
- Reduce the digoxin dose by 50% (or 33% if kidney function is poor).
- Order a repeat digoxin level in 72 hours.
- Monitor for nausea, vision changes, dizziness, or irregular heartbeat.
- Reassess every week for the first month.
What About Other Drugs?
Amiodarone interacts with dozens of medications - warfarin, statins, beta-blockers. But none carry the same immediate, life-threatening risk as digoxin. The digoxin-amiodarone combo is unique because:- The therapeutic window is tiny.
- The mechanism is well understood.
- The fix is simple and immediate.
- The consequences of inaction are deadly.
How soon after starting amiodarone does digoxin toxicity occur?
Digoxin levels typically begin rising within 24 to 48 hours of starting amiodarone, with peak levels occurring between 1 and 2 weeks. However, toxicity symptoms can appear as early as 3 days. That’s why checking digoxin levels at 72 hours is critical - waiting longer increases the risk of serious complications.
Can I just monitor digoxin levels without reducing the dose?
No. Waiting to reduce the dose until levels are high is dangerous and reactive. Studies show that even patients with initially normal digoxin levels experience a 100% increase in serum concentration after amiodarone starts. Proactive dose reduction by 50% is the only safe approach. Monitoring alone is not enough.
What if the patient is already on a low digoxin dose?
Even low doses can become toxic. For example, if a patient is on 0.125 mg daily (a low dose), reducing it by 50% means switching to 0.0625 mg daily - which is still a standard, safe dose. Never assume a low dose is safe with amiodarone. Always reduce.
Does this interaction happen with dronedarone too?
Yes. Dronedarone, a newer drug similar to amiodarone, also increases digoxin levels. The PALLAS trial showed a 31% higher risk of cardiovascular death when dronedarone was added to digoxin. The same 50% dose reduction rule applies. Don’t assume dronedarone is safer in this context.
How long does the interaction last after stopping amiodarone?
Amiodarone and its active metabolite can remain in the body for up to 60 days after discontinuation. This means digoxin levels may stay elevated for weeks. Never increase the digoxin dose immediately after stopping amiodarone. Wait and monitor levels before adjusting.
Is digoxin still used today, or should it be avoided entirely?
Digoxin is still used, but only in specific cases - mainly heart failure patients with reduced ejection fraction who don’t respond to other therapies. For atrial fibrillation, guidelines now prefer beta-blockers or calcium channel blockers for rate control. If amiodarone is needed, avoid digoxin if possible. But if digoxin is essential, use it cautiously - with strict dose reduction and monitoring.
