A cerebral aneurysm isn’t something you hear about until it’s too late. It’s a weak spot in a blood vessel in your brain that balloons out like a tiny blister. Most people never know they have one - until it bursts. And when it does, the consequences can be sudden, devastating, and often fatal. About 3.2% of people worldwide have at least one unruptured aneurysm, but only about 1 in 10,000 will have it rupture each year. Still, when it happens, 30 to 40% of people die within the first 24 hours. That’s why understanding your risk - and what can be done - matters more than you think.
What Makes a Cerebral Aneurysm Rupture?
Not all aneurysms are created equal. Some stay small and harmless for decades. Others burst without warning. The difference comes down to a mix of things you can’t change - and things you can.
Age is a big one. If you’re over 65, your risk of rupture is more than double compared to someone in their 40s. Women are also more likely than men to develop them, and if you have two or more close relatives who’ve had one, your risk jumps fourfold. Genetics matter. But here’s the thing: even if you’re in a high-risk group, you’re not doomed. Many aneurysms never rupture.
The real danger comes from lifestyle. High blood pressure is the biggest modifiable risk. If your systolic pressure stays above 140 mmHg, your rupture risk goes up by 2.3 times. Smoking? It’s even worse. Current smokers have over three times the risk of non-smokers. And if you smoke more than 10 cigarettes a day? Your risk climbs by nearly half. Heavy drinking - more than 14 drinks a week - adds another 32% to your chances.
Then there’s the shape and size of the aneurysm itself. Size matters. Aneurysms 7 mm or larger have over three times the risk of rupture compared to smaller ones. But shape is just as important. If it’s irregular, has a daughter sac (a smaller bulge off the main one), or looks more like a lopsided balloon than a round bubble, your risk spikes. Aneurysms in certain spots - like the anterior communicating artery - rupture more often, even if they’re small. Some as tiny as 4 mm in that area have broken open.
It’s not just about looks. Blood flow inside the aneurysm plays a role too. If the blood swirls unevenly or presses weakly on the wall, it wears down the tissue over time. Studies show 83% of ruptured aneurysms had abnormal flow patterns, compared to just 42% of unruptured ones. Inflammation inside the wall, triggered by genes and immune responses, also weakens the vessel. People who rupture often have higher levels of IL-6 and CRP - markers of inflammation - in their blood.
How Do Doctors Predict Rupture Risk?
Doctors don’t guess. They use tools. The most trusted one is the PHASES score is a validated risk model that combines Population, Hypertension, Age, Size, Earlier subarachnoid hemorrhage, and Site to estimate a patient’s 5-year rupture risk. It gives you a number from 0 to 10. A score of 0-3 means your risk is under 3%. A score of 9-10? That’s a 45% chance of rupture in five years.
Each point you earn raises your risk by 32%. So if you’re over 65, have high blood pressure, and your aneurysm is 8 mm, you’re already at 6 or 7 points. That’s the tipping point. Most guidelines say if your PHASES score is 6 or higher, treatment should be considered.
Another tool, the ELAPSS score is a 1-year risk predictor based on Earlier SAH, Location, Age, Previous SAH, Size, and Shape, helps when you need a shorter-term view. And for aneurysms that are growing, the triple-S model is a prediction tool using Size, Site, and Shape to estimate rupture risk over 6 months, 1 year, or 2 years works well - it’s accurate enough to be used in clinical decisions.
Multiple aneurysms? That’s another red flag. Having more than one increases your rupture risk nearly fourfold. And if you’ve already had one rupture? Your chance of another is over five times higher.
Treatment Options: Clipping, Coiling, and Flow Diversion
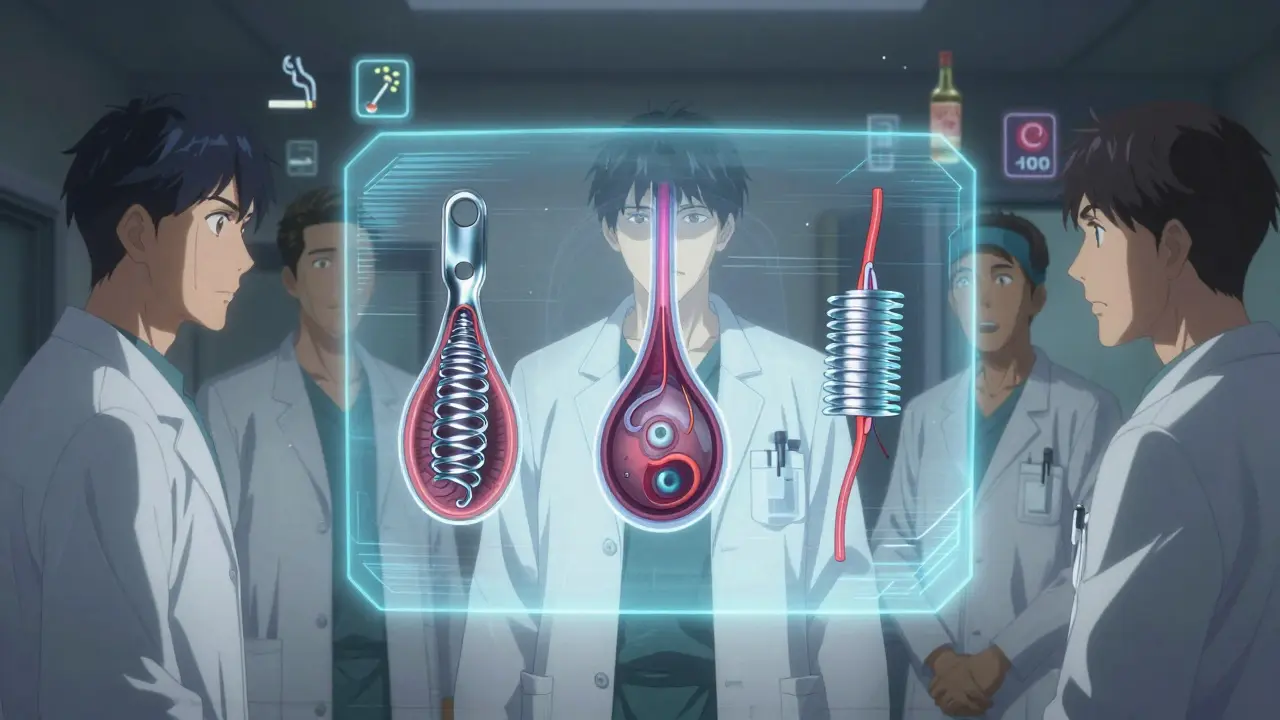
If your aneurysm is high-risk, doctors will talk about treatment. There are three main options - each with pros, cons, and ideal candidates.
Microsurgical clipping is the oldest method. A neurosurgeon opens your skull, finds the aneurysm, and places a tiny titanium clip across its neck. This cuts off blood flow to the bulge. It’s been done since 1937. Success rates are high: 95% of clipped aneurysms are fully sealed. The cure is permanent - only 8-12% need retreatment. But it’s invasive. Recovery takes weeks. Complication rates? About 4.7% permanent disability and 1.5% death. It’s often used for aneurysms in hard-to-reach spots or those with wide necks.
Endovascular coiling is less invasive. A catheter is threaded from your groin up to the brain. Platinum coils are pushed into the aneurysm, triggering a clot to form and seal it off. First done in 1991, it’s now the most common treatment. At six months, 78-85% are fully blocked. Recovery is faster - most people go home in a day or two. But it’s not always permanent. About 16% need another procedure within 12 years. The ISAT trial is a landmark study showing endovascular coiling reduced 1-year mortality by 22.6% compared to surgical clipping (8.1% vs 10.1%).
Flow diversion is the newest. Devices like the Pipeline Embolization Device is a porous stent placed in the artery to redirect blood away from the aneurysm, allowing it to heal over time act like a sieve. Blood flows through the stent, bypassing the aneurysm. Over months, the aneurysm fills with clot and shrinks. It’s especially good for large or giant aneurysms, or those with wide necks. The WEB (Woven EndoBridge) is a device approved in 2019 for aneurysms at branch points in the brain, with 71.4% complete occlusion at 1 year is another option for tricky spots. Success rates? Around 76-85% at one year. Mortality is low - just 0.8% - but complications like stroke or bleeding can happen in 5.2% of cases.
Who Gets Which Treatment?
You don’t pick. Your team does - based on your anatomy, age, and health.
Clipping is often chosen for:
- Aneurysms in the posterior circulation (back of the brain)
- Patients under 60 with good overall health
- Wide-necked aneurysms that won’t hold coils
Coiling is preferred for:
- Patients over 70
- Those with other health problems like heart disease
- Aneurysms in the front of the brain
Flow diversion works best for:
- Giant aneurysms (over 25 mm)
- Aneurysms that failed coiling
- Complex shapes that can’t be treated with coils alone
Age changes everything. Patients over 70 have 35% higher surgical risks. Hypertension raises perioperative complications by 28%. If you’re diabetic, have kidney disease, or smoke, your chances of problems go up. That’s why doctors weigh not just the aneurysm - but your whole body.
What If You Don’t Treat It?
Many small aneurysms - especially under 5 mm - are watched, not treated. The UCAS Japan study is a large study showing that unruptured aneurysms under 5 mm had only a 0.2-0.7% 5-year rupture risk. That’s lower than the risk of surgery for many people.
Monitoring means regular imaging - usually an MRA scan every year. If it grows, changes shape, or your PHASES score climbs, treatment kicks in.
Medical management is just as important. Controlling blood pressure to below 130/80 mmHg cuts rupture risk. Quitting smoking reduces risk by over half within two years. Cutting back on alcohol helps too. No medication can shrink an aneurysm - but lifestyle changes can stop it from exploding.

What’s Next? The Future of Prediction and Treatment
Science is getting smarter. The HUNT study is a long-term research project identifying 17 genetic markers linked to aneurysm formation and rupture is helping us find who’s most at risk before they even have symptoms.
Machine learning is being trained on hundreds of data points - shape, flow, wall thickness, inflammation markers - to predict rupture better than any score ever could. One model using 42 variables is already outperforming PHASES.
New devices are coming. Smaller, more flexible flow diverters. Biodegradable coils. Nanotech that targets inflammation inside the wall. These won’t be mainstream for years - but they’re coming.
Right now, the best defense is knowing your risk. If you’ve got a family history, high blood pressure, or smoke - get screened. If you’re found to have one, don’t panic. Most won’t rupture. But if yours is high-risk? Treatment works. And the right choice can mean the difference between life and death - or between recovery and permanent disability.
Key Takeaways
- 3.2% of people have unruptured brain aneurysms - most never cause problems.
- Size over 7 mm, irregular shape, and location (like AComm artery) are major rupture triggers.
- Smoking, high blood pressure, and heavy drinking each multiply your risk by 2-3 times.
- The PHASES score is the gold standard for deciding whether to treat or monitor.
- Clipping, coiling, and flow diversion are effective - but choice depends on age, health, and aneurysm shape.
- Quitting smoking cuts rupture risk by 54% in two years. Blood pressure control is essential.
Can a cerebral aneurysm go away on its own?
No, a cerebral aneurysm does not heal or disappear without treatment. Once formed, it remains a weak spot in the artery wall. In rare cases, a small aneurysm may clot off naturally, but this is unpredictable and not reliable. Monitoring or medical intervention is still needed to prevent rupture.
Is screening for cerebral aneurysms recommended for everyone?
No, routine screening isn’t recommended for the general public. It’s only advised for people with two or more first-degree relatives who’ve had a ruptured aneurysm, or those with certain genetic conditions like polycystic kidney disease or connective tissue disorders. For most people, the risks of unnecessary testing outweigh the benefits.
How long does recovery take after aneurysm treatment?
Recovery varies by treatment. After coiling or flow diversion, most patients return to normal activities in 1-2 weeks. Surgical clipping requires a longer recovery - typically 4-8 weeks - because it involves opening the skull. Full healing can take months, especially if there was a rupture before treatment.
Can stress or exercise cause an aneurysm to rupture?
Extreme physical strain - like heavy lifting or intense anger - can briefly spike blood pressure and increase rupture risk. But regular moderate exercise is safe and even helpful. The real danger is uncontrolled high blood pressure, not daily activity. Always consult your doctor before starting a new exercise routine if you have an unruptured aneurysm.
What are the chances of an aneurysm coming back after treatment?
After successful clipping, recurrence is very rare - less than 10%. With coiling, about 16% need retreatment within 12 years because the aneurysm can refill. Flow diversion has low recurrence rates - under 5% - because it reshapes blood flow long-term. Regular follow-up imaging is essential for all treatments.
If you’ve been told you have an unruptured aneurysm, remember: this isn’t a death sentence. It’s a warning sign - and one that can be acted on. With the right information, monitoring, and care, most people live full, normal lives.
